
Redundancy, duplication, and waste. They are pervasive in today’s healthcare delivery system, driving up operating and capital costs. And in an era of increasing consolidation, healthcare organizations that expand through mergers and acquisitions are increasingly challenged to operate as a unified system—and often face painful decisions about redundant service offerings.
To achieve economic sustainability and market essentiality, we believe health systems must integrate and rationalize to enhance clinical care, optimize operations, and lower costs, ultimately focusing on the improvement of every aspect of patient care operations.
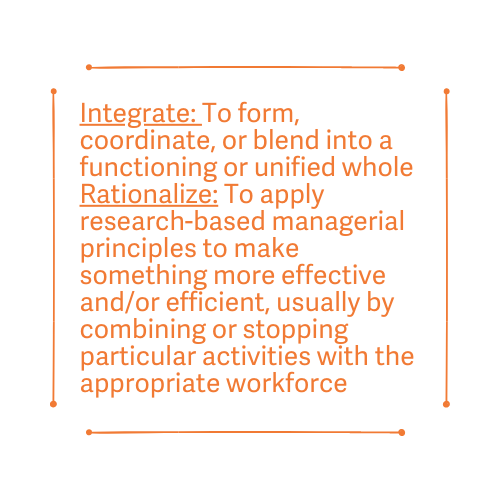
For hospitals and health systems, integration might mean implementing common operational processes and workflows, adopting evidence-based protocols and clinical pathways, and approaching decision-making with a system mindset. Rationalization is more likely to centralize corporate functions or alter the scope, mix, and/or distribution of clinical services.
Pursuing integration and/or rationalization is difficult, as both call for examining and typically changing what is being done where and by whom. Healthcare leaders encounter internal hurdles—culture, leadership commitment, and resources—and external obstacles, in the form of community resistance, local political pressure, and state-specific regulations. Little wonder that many organizations have been slow to start down this path.
Industry Trends Increase the Urgency
The financial repercussions of the COVID-19 pandemic, particularly the increased expenses associated with premium labor and supply costs, are compelling more health systems to find ways to enhance the efficiency of their back-office functions and care delivery processes. But even before the impact of COVID-19 was widely felt, several industry trends were causing provider organizations to examine the need to integrate and/or rationalize.
- An aging population: With about 10,000 people turning 65 every day, hospitals are finding Medicare accounting for a greater percentage of patient revenue. The change in payer mix makes it harder use margins from commercial business to offset losses on Medicare and Medicaid.
- Regulatory and pricing pressures: As CMS allows more procedures to be performed in outpatient settings, surgery migration to freestanding ASCs is accelerating. The growth of digital health will also require providers to reexamine care delivery location options.
- Alternative payment models: Success under risk-based pricing models requires close examination of clinical and operations processes to identify opportunities to reduce unnecessary utilization, minimize clinical variation, and eliminate waste.
- Care delivery and workforce changes: Site-of-care shifts, fewer avoidable admissions, and lower readmission rates mean that tomorrow’s hospitals will be occupied by high-acuity patients and those requiring complex, specialized diagnostic and therapeutic procedures. The aging workforce and projected shortage of providers are also forcing health systems to rethink how and where care is delivered.
Given these trends, health systems should focus on the following four imperatives to realize the benefits of integration and rationalization.
1. Capitalize on Technology Innovation for Business Tasks
Many health systems have already adopted integrated revenue cycle operations that centralize people and standardize processes. But recent technology innovations bring new opportunities to drive cost savings while improving the consumer experience.
- Access and scheduling: Digital tools allow consumers to schedule appointments and complete preregistration on their computer or mobile device.
- Revenue cycle: AI and robotic process automation offer opportunities to reduce redundancies and improve productivity throughout all aspects of the revenue cycle, freeing up administrative staff to focus on tasks that require complex interaction and decision-making.

2. Eliminate Unwarranted Clinical Variation
Unwarranted clinical variation can be defined as resources expended in services, money, time, and/or personnel that do not add value. This variation often exists because departments across sites of care have different operational processes and workflows, there aren’t agreed-upon evidence-based protocols for delivering care, and/or individual physicians use different medical and surgical supplies and patient care philosophies.
Foundational elements for addressing unwarranted clinical variation include the following:
- Standardized clinical and operational processes: Developing and implementing uniform, evidence-based protocols and pathways across the system establishes one model of care and greater consistency across sites.
- Technology: Clinical decision-support tools integrated into the EHR equip clinicians with actionable, real-time clinical and financial data to make more informed patient care decisions, and alerts can help reduce unwarranted clinical variation and unnecessary or duplicative tests.
- Physician engagement: Without strong physician alignment, initiatives to reduce unwarranted clinical variation, standardize operational processes, and adapt to new technology will have limited chance of success.

3. Design a Platform for Delivering and Coordinating Care across the Continuum
The care delivery platform for an integrated and rationalized health system looks dramatically different than what is in place at most organizations today. Transitioning to this platform requires:
- Operating as a single entity: Despite significant consolidation of hospitals and physician practices over the past decade, few organizations make the tough decisions about integrating and rationalizing operations and services. As a result, most health systems stop short of achieving many of the potential strategic and operational benefits. Regardless of a health system’s corporate structure, functioning as a single operating entity is essential. Implementing one model of care with standardized clinical protocols and consistent operational processes will break down operational silos.
- Aligning with physicians: To create a network in which patients receive the right care in the appropriate setting, health systems will need to achieve clinical and financial alignment with the physician community. Health systems can pursue a range of formal alignment options, including comanagement agreements, joint ventures, and clinically integrated networks and accountable care organizations.
- Rationalizing clinical services to optimize resources: As it becomes increasingly difficult for health systems to meet all of the healthcare needs of their communities, more organizations will need to rethink, and potentially rationalize, the clinical services they provide. Consolidating services, or eliminating them entirely, are difficult decisions but may be the only way to remain viable and continue serving the community in some capacity.
4. Implement a Capital Asset Plan That Supports Integration and Rationalization
Going forward, capital asset strategies and associated investments will need to provide the underpinning of an integrated, rationalized, efficient delivery system.

- Rationalize current capital assets: Health systems should conduct an assessment to determine the best short-term and anticipated future uses of available capital assets. Establishing which facilities require upgrades, can continue operation with maintenance, should be repurposed, and should be phased out will increase revenue and decrease costs in the long run.
- Build adaptable and flexible facilities: Ambulatory care sites should be built to accommodate multiple clinical service lines, diagnostic and therapeutic services, and physicians and specialists on any given day. Similarly, inpatient rooms should be designed with the flexibility to quickly transition to ICU capabilities when needed.
- Develop an integrated technology ecosystem: Patients are increasingly engaging with providers via telemedicine, remote diagnostic and therapeutic procedures, and online portals. The transition to new access channels changes facility and space needs for health systems, reinforcing the importance of building flexible, adaptable spaces.
Is your organization prepared for the changing trend?
This blog post is excerpted from part one of our We Believe series, a collection of strategic perspectives on the changing dynamics of the US healthcare system.

