
Academic and community healthcare providers are still too often trying to position themselves as winners in a competition for patients rather than as collaborators in population health. The result has historically been duplicative investments despite geographic alignment and shared patient populations.
In Nashville, for example, an academic medical center, a community hospital and a for-profit hospital each offer transcatheter aortic valve replacement (TAVR). The procedure, which targets a small population of qualified patients, requires a multidisciplinary team of specialists and a hybrid operating room that costs $3 million to $4 million. And in the Washington, D.C., region, changes to proton therapy reimbursement have spurred an arms race for a technology that can cost more than $100 million to implement.ii Across the country in the Northwest, the region’s hospitals have 12 CT scanners among them, with more in private offices, to serve a population that would need only eight even if it grew by 25%.
The well-intentioned investments in less-invasive procedures have the potential to achieve the triple aim, but only so much: If teaching hospitals and community healthcare systems can overcome their historic divisions to resolve longstanding turf wars and create efficiencies, the impact on future healthcare delivery will be even more significant. If they can’t, they leave themselves open not just to unsustainable costs, but to outside competition. Flooding the market with costly infrastructure is a losing strategy, particularly as innovation in digital health and telemedicine continues to increase the number of virtual healthcare access points in patients’ homes and communities.
The logical starting place for AMC and community health provider collaboration is to form partnerships around specific clinical service lines and disease groupings.
While providers must deploy digital solutions in the future, the logical starting place for academic medical center (AMC) and community health provider collaboration is to form partnerships around specific clinical service lines and disease groupings. Partnering to transform care delivery offers the greatest opportunity for population health progress: Outcomes can be improved and costs lowered by cultivating synergies in both organizations’ traditional core competencies and by sharing infrastructure to create more efficient delivery platforms.
Erasing the Line Down the Middle
The tension between AMCs and community hospitals has largely stemmed from their different missions. The former take on the costs of teaching new physicians and translate research into innovative clinical care delivery, while the latter tend to provide convenient and efficient care that meets communities’ more general healthcare needs.
Fundamentally, in a population health paradigm, both seek to increase value and prove that their own value propositions are legitimate. Service line collaboration allows the partnership, and the required trust among providers, to develop. Efficiencies and cultural cross-pollination can eventually scale up to encompass more services or to the mutual pursuit of risk-based contracts, bundled services and other value-based care delivery approaches.
Selecting a Middle Ground
To effectively drive outcomes, clinically integrated service lines coordinate patient care across all care settings, from screening and prevention to end-of-life care. In particular, service lines like cancer, which are highly fragmented and multidisciplinary, present a significant opportunity for mutual benefit. Potential partners should focus on identifying a service line that each entity offers in a slightly different way or to a different audience and find synergies that reduce the cost of care, improve care transitions, ensure that care is delivered in the appropriate setting, improve access to subspecialists and otherwise advance the triple aim.
In many cases, these initial partnership opportunities open the door for future integration of services in areas where cultural or historical perceptions are major barriers
Or they can focus on services that neither partner yet provides but both want to provide in the future. These are commonly non-revenue-generating supportive care services like financial counseling, patient navigation and patient registries. They could also be community need–based services like rehabilitation and psychosocial services. Joint fundraising around these new service lines allows teaching and community hospitals to pool resources toward improving a program or delivery model without spreading themselves too thin. It’s also a good start toward integrating planning.
In many cases, these initial partnership opportunities open the door for future integration of services in areas where cultural or historical perceptions are major barriers. Initially, potential partners should move on quickly from more difficult options to find common ground where opportunity exists to collaborate. These areas include information technology, telehealth, scheduling and other back-office needs, outpatient network development, and community education programs that can serve as footholds into deeper academic-community relationships.
(Service) Lines in the Sand
Promising collaborations are occurring in cancer care and cardiac care. Both provide more natural delineation than other service lines as to which provider does what along the care continuum. High-complexity, invasive care can be centralized in a higher-acuity setting, while lower-acuity care, follow-up and prevention can be owned by community providers along the continuum.
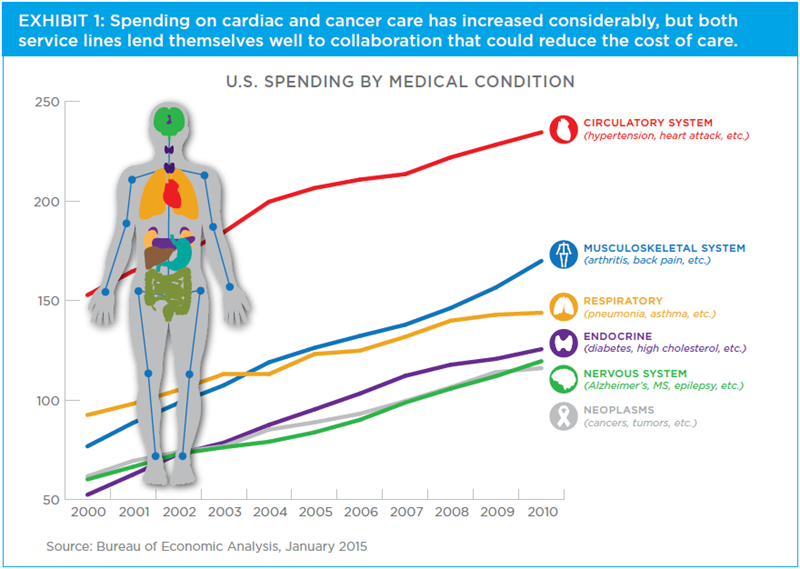
Further, both service lines account for a large portion of costs nationally. (See Exhibit 1.) Considerable room exists to coordinate efficiencies, reduce duplication, lower the cost of care and drive business growth—community providers could care for a lower-acuity market share that is currently provided at the AMCs, and AMCs, in turn, could backfill with higher-margin, higher-acuity patients. Additionally, patients benefit by receiving a consistent patient experience, better integration across delivery settings and increased access to the optimal care team.
Shared service line models succeeding thus far also have, at least at their starting point, an opportunity to grow the service. In one Northeastern city, the academic cancer provider and the regional community health system joined forces under a comanagement agreement to jointly recruit physicians, invest in expanded clinical trial infrastructure and outpatient cancer services, and provide a more cohesive and coordinated cancer program. This cooperative includes a shared governing body that advances the common goals of the partnership and strives to improve quality and reduce duplication of expensive services.
In one Southeastern city, synergies were identified in women’s cancer services. A tertiary teaching hospital, a women’s hospital and a community cancer care provider partnered to create a women’s cancer program. Common goals were developed, with a separate joint affiliation entity whose sole responsibility was to advance shared goals—not to promote one facility or another. The entity shares common care models and philanthropic efforts and also consolidated functional areas to reduce overhead, including supporting care services that are critical to patient quality of life but lack a reimbursement component.
Who Rules in Neutral Territory?
These affiliations often include a separately governed entity. In some cases, a sole employee, an administrator, is funded by the partners. But leadership must also be mobilized at both the academic facility and the related community facilities. Coordination will require cross-functional teams that represent each partner to develop patient pathways and care protocols that work seamlessly across partners and that incentivize cost-effective care. So will quality: In one study on cardiac care, heart attack mortality rates were 33% higher in hospitals with less-evident cross-continuum coordination and communication.
In California, an academic medical center is working with several community hospitals to develop a system of care that relies on multiple types of physician incentive programs. Having acquired several physician practices, they’ve chosen not to place academic physicians in those satellite facilities, instead establishing community incentive models that tend to be more value-driven and cost-sensitive, while keeping faculty at the main campus.
Cross-partner physician leadership is critical in such efforts. At the same California AMC, a newly hired oncologist with considerable experience in both community-based and AMC-based cancer care has been instrumental in developing relationships among community-based physicians and a breast care team of oncologists and plastic surgeons. This collaborative approach contributed to 40% growth of the program from 2010 to 2013.
Happy Medium
Consolidation alone doesn’t create efficiency. It takes enhanced working relationships and collaboration, as well as deployment of physician incentive structures that drive care delivery to the most efficient settings. Blending academic and community healthcare delivery won’t be easy. But if providers can get enough synergies funded in a common manner, and build strength around that, they can create a meaningful budget for a new, shared entity.
Key is the creation of an entity that represents the collective vision, an entity governed by an advocate for the collaborative goals and empowered by a shared budget.

