During the past 5 years, cardiologists have experienced a large increase in hospital and health system employment. While greater alignment promised substantial opportunities for increased care coordination, service line development, and improved outcomes, these benefits have often been elusive. Health systems are facing challenges related to financial sustainability and performance, due partly to lucrative cardiology deals that lack underlying incentives for performance. Provided here are three steps that organizations can take to enhance productivity, operational performance, and long-term financial viability for their integrated cardiology service line.
Step 1: Ensuring Efficient Operations
In the early stages of employment, cardiology practices are often promised that they can operate similarly to their pre-integration days, which is typically not the most efficient way to manage a group. The recruitment of a skilled cardiology practice manager who will closely monitor service line performance is a key overarching step to ensure that major opportunities and/or issues will be quickly addressed. While each organization is unique, some of the more common challenges include:
- Scheduling patient visits to maximize provider time. This is especially important in a specialty such as cardiology, given cardiologists’ extensive outreach time and complicated call schedules. Carefully monitoring physicians’ schedules, including vacations, helps ensure that the clinic is appropriately covered at all times.
- Properly staffing the clinic and hospital. Practices are frequently either understaffed or overstaffed, particularly for a specialty such as cardiology, where their historically integrated services are often separated into multiple departments under an employed arrangement. Additionally, staffing could be better leveraged in both the outpatient and inpatient settings (e.g., the use of an MA instead of an RN).
- Maximizing revenue cycle operations. Opportunities typically exist for revenue cycle improvements, despite the best of intentions. From the physician perspective, a cardiology practice can often achieve productivity improvements simply through coding education and more thorough documentation, particularly in the hospital setting.
- Monitoring performance and routinely sharing results with the physicians. Creating performance dashboards allows managers and physicians to monitor key metrics, such as WRVUs and staffing expenses, on a regular basis. This can prove challenging for a cardiology service line, since it typically spans multiple departments of a hospital; however, even a simple Excel report can help influence behavior and build rapport.
Step 2: Creating the Optimal Care Model
To maximize efficiency, cardiac programs are also beginning to leverage CV-specific care team models, typically consisting of two physicians and an advanced care practitioner (ACP). Assigned to a panel of patients, this team model allows for more efficient follow-up scheduling and a greater sense of continuity. Once the initial operational challenges have been addressed, the team of three providers can expect to increase its panel size.
Patients generally prefer obtaining a timely appointment with an ACP that includes a brief visit with their physician to waiting for a full appointment with the physician. Also, if used effectively, a cardiac ACP may generate 2,500 to 3,000 WRVUs per year. One ECG client reported that this approach allows a physician and ACP to see as many as 35 to 38 patients combined in a day, which represents a substantially more productive practice than even the most recognized national cardiology programs.

Step 3: Aligning Incentives With Cardiology Service Priorities
A primary factor in financial sustainability is an organization’s compensation plan design. Though many cardiology groups incorporate a productivity-based component into their compensation plans, the base is often set too high and physicians do not hit the incentive. Additionally, the negotiated terms frequently incorporate a high payment rate that is unrealistic, given current practice economics and reimbursement trends. According to industry surveys, cardiologists’ compensation per WRVU has increased during the last 3 years, despite a decrease in collections per WRVU. This trend is obviously not sustainable.
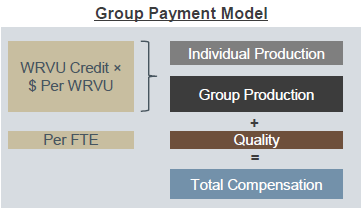
Consequently, an increasing number of organizations are adopting compensation plans that put more dollars at risk for both production and nonproduction service line performance (e.g., quality). This methodology is not exclusive to employed medical groups, yet the payment approach offers a unique set of challenges for cardiology in light of operational dynamics regarding cardiac diagnostic imaging, hospital call coverage requirements, outreach, etc. While these services are important for a robust cardiology practice, the most efficient model is not necessarily that which generates the most WRVUs. Many hospitals and physicians opt for a group compensation methodology, whereby the physicians are paid – at least in part – for their collective productivity and overall performance. For example, some organizations opt to have a physician dedicated each day to reading all interpretations, while another physician provides hospital coverage. Under this group compensation model, each physician would be compensated commensurately for his/her work – regardless of the WRVU productivity differential – by allocating a large amount of compensation to a group production pool, as illustrated in the example above.
Preparing for Future-State Trends
Recent opinions from MedPAC and others suggest that additional cuts for cardiology services may be imminent. Consequently, it will become even more important to monitor cost-saving measures and identify potential efficiencies. The mechanisms described above are just some of the approaches that organizations are using to mitigate downward reimbursement trends and achieve performance improvement goals. However, the efficacy of these mechanisms relies on organizations’ ability to clearly define and track service line performance, an endeavor that is especially important for a specialty such as cardiology that often spans multiple departments and/or cost centers (e.g., diagnostics, nursing, rehabilitation). To fully realize the benefits of an employed cardiology group, it will be important for organizations to dedicate sufficient resources to this effort and to ensure that all service line leaders have timely and accurate data related to service line performance.

