
Digital health has become an essential way for physicians to continue caring for their patients while reducing the risk of exposure to contagious diseases. Remote patient monitoring (RPM) of chronically ill patients or those needing monitoring for COVID-19 adds patient convenience and safety to the peace of mind that comes from knowing that potential worsening health conditions can be caught while still manageable.
As an added benefit, with 97% of physician practices experiencing a negative financial impact from COVID-19,[1]RPM provides a new revenue stream to help medical groups offset lost revenue.
In the 2020 MPFS Final Rule, CMS defines RPM as the “collection, analysis, and interpretation of digitally collected physiologic data, followed by the development of a treatment plan, and the managing of a patient under the treatment plan.”
- Chronic Conditions: CHF, diabetes, COPD
- Post-Acute Care: posthospital admission or postsurgical treatment
- COVID-19: suspected and confirmed cases
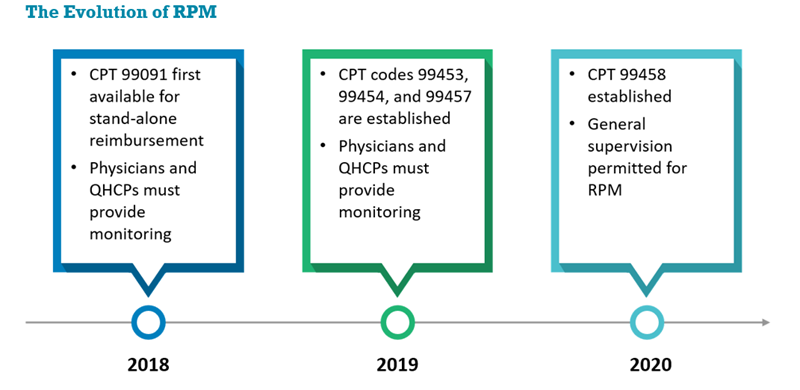
Starting in 2018, RPM was separately reimbursable via CPT code 99091. Thirty minutes of time with either a qualified healthcare professional (QHCP), such as an advanced practice professional, or a physician was required over a 30-day period to bill for RPM.
In 2019, three new CPT codes—99453, 99454, and 99457—were established. This was a significant change, as it meant physician practices would be reimbursed for the time they spent educating patients and the devices used for RPM (e.g., blood pressure monitor, glucose monitor). Two other key changes also occurred: in addition to QHCPs and physicians, clinical staff were also permitted to monitor patients, and only 20 minutes of time was required per month instead of 30. Despite these advancements, one important barrier remained—both QHCPs and clinical staff required direct physician supervision to bill for 99457.
Effective January 1, 2020, CMS made two more significant changes:
- Permitting general supervision, instead of direct supervision, to bill for 99457
- Adding CPT code 99458 to reimburse providers when patients require an additional 20 minutes of monitoring in a month
It is important to note that 99091 and 99457 cannot be billed simultaneously.
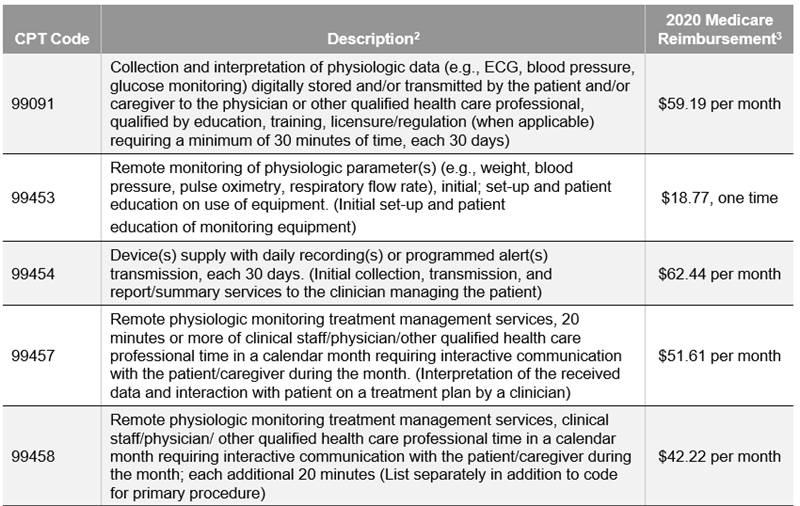
A summary of the CPT codes discussed, and their reimbursement, can be found below.
RPM: A New Revenue Stream
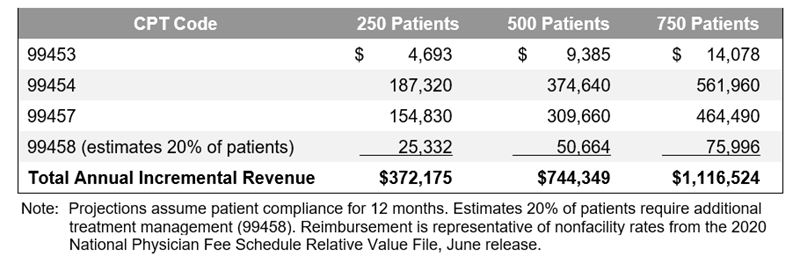
RPM can provide significant incremental annual revenue, as shown in the table below, particularly as it is scaled across an organization.
Key Considerations for Implementation
Organizations need to consider four main factors as they contemplate implementing RPM:
- Financial Opportunity: Calculate the financial opportunity of RPM by estimating the number of participating physicians and eligible patients. It is important to remember that not all participating patients will meet the time threshold of 20 minutes under 99457. Additionally, determine potential reimbursement for commercial, Medicare Advantage, and Medicaid patients. You will also need to consider the degree to which the additional revenue will be offset by the cost of implementation.
- Impact on Value-Based Contracts: While RPM is an additional revenue source in a fee-for-service world, it is also an additional claims expense that would be added to the total cost of care under a value-based contract arrangement. On the other hand, you will likely realize more value from a potential reduction in ED visits, avoidable admissions, and readmissions.
- Technology Selection: Two key technology selections are required:
- Equipment: Identify the most appropriate RPM advice for your organization and patients. To offset the equipment for Medicare members, CMS will reimburse physicians $62.44 per month via CPT code 99454.
- RPM Software: Select the RPM software that will integrate with the selected technology and allow for monitoring patients remotely.
- Vendor Selection: Evaluate your infrastructure, the operational planning required, and the level of work you want to take on to determine the degree of outsourcing that makes sense for your organization. You can select a vendor for the technology platform or choose an RPM vendor for the entire process, including the initial setup of the device with patients as well as provision of RNs and medical assistants to monitor patients. If you opt for a vendor, identify and research potential RPM vendors and orchestrate an RFP process. RPM vendors can often get an organization up and running on an RPM platform in just a few weeks.
If it makes sense for your organization, we encourage you to take advantage of RPM.
Footnotes
1. [1] Information obtained from https://www.healthleadersmedia.com/finance/97-physician-practices-take-covid-19-financial-hit, originally citing a 2020 MGMA survey.
2. [2] Descriptions obtained from the AMA at https://www.ama-assn.org/system/files/2018-12/playbook-resources-step-5-coding-payment-REV1.pdf and https://www.ama-assn.org/system/files/2020-05/covid-19-coding-advice.pdf.
3. [3] Reimbursement is representative of nonfacility rates from the 2020 National Physician Fee Schedule Relative Value File, June release.

