
In their attempt to control costs and monitor clinical care and outcomes, payers have increased the volume of claims denied for initial payment. This denials deluge has caused significant strain on provider organizations’ operational and financial performance. Successfully addressing the increase in payer denials requires provider organizations to establish internal collaborative processes to identify trends, prioritize and escalate concerns, and aggressively manage payers in resolving issues. Only by collaborating internally can provider organizations get back on track.
Developing a Collaborative Approach
The information included on any billed claim reflects contributions from many departments: patient access, coding/HIM, providers, etc. These departments must also contribute to an organization’s denials management strategy, which should start with the development of a cross-functional denials-management committee. This committee should be tasked with developing comprehensive denial-mitigation strategies, and should include representatives from the following:
- A/R management
- Patient access
- Revenue integrity
- Coding
- Information systems
- Case management
- Managed care
Committee meetings should feature templated denial reports with key metrics trended over time to show performance improvement or decline. These reports will guide the meeting and inform non–revenue cycle departmental stakeholders of denial root causes within their respective areas. In addition to standard reporting, leading provider organizations are starting to invest in artificial intelligence to identify microscopic trends that may be masked by macroscopic issues. Robotic process automation is another growing technological solution that is reducing manual intervention across a variety of processes, increasing data quality and preventing downstream denials. These tools are also beneficial in keeping payers actively engaged by providing data to highlight improvement opportunities as well as opportunities to partner with them to build and monitor systematic solutions that will prevent future denials.
Coordinate Closely with Managed Care
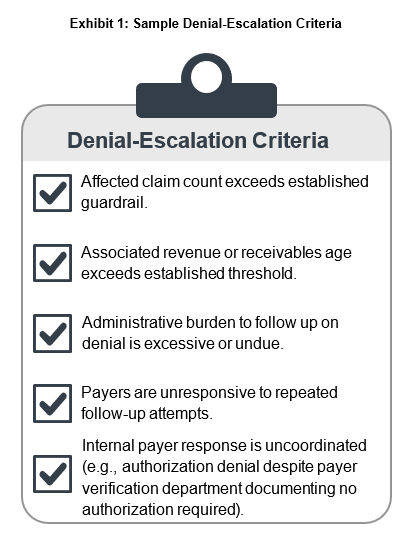
Beyond the denials committee, revenue cycle should develop a close partnership with managed care to systematically address and reduce denial volumes. Managed care’s role leading contract negotiations strategically positions it to support denial management. Managed care leaders have relationships within the payer organization to provide an escalation path when follow-up efforts are ineffective. Revenue cycle and managed care should establish criteria to determine when operational or claims-payment issues require escalation (see exhibit I). These guardrails will support a proactive and collaborative approach to resolving issues as they arise.
Bulk Issue Resolution
As denial trends are identified, follow-up should be escalated to initiate appeal projects aimed at resolving, through payer representatives, multiple denials based on a common issue. Appeals projects should include resolution of both the root cause of the denials and the associated backlog of unpaid claims. To fully close the project, organizational leaders should work with the payer to update payer system edits to prevent future denials for the same problem.
Joint Operating Committees (JOCs)
One common approach is for provider organizations and payers to maintain regular communication through JOCs. Typically this involves a series of recurring meetings or phone calls that address and resolve operational and contractual problems. JOCs can provide a collaborative forum for addressing outstanding issues and developing strategies to resolve them. These meetings should be tightly managed to ensure emphasis is consistently placed on progress, not solely on identification or tracking. Progress can be challenging based on payer-representative turnover and slow payer response to the issues escalated.
The JOC is also an effective forum for escalating Division of Financial Responsibility (DOFR) payment challenges. Payer representatives should be engaged to obtain a copy of the payer DOFR that includes billing code–level detail that provider organizations can use to more definitively identify the assignment of financial liability. While payers may be reluctant to provide this level of transparency, managed care leaders should continually advocate for it.
Payer Scorecards
Managed care should lead the development and oversight of a payer scorecard to monitor each payer’s performance against their assigned contract. The scorecard should include feedback from revenue cycle on denial trends and any operational issues raised by other departments. Scorecards provide a common set of metrics to benchmark payers and provide an at-a-glance summary of payer strengths and pain points for use during JOC meetings and contract negotiations.
Contract Negotiations
Beyond day-to-day denial management, contract negotiations provide an important opportunity to resolve denial issues. Managed care leaders should work closely with their revenue cycle counterparts prior to contract negotiations to understand the latest denial patterns and incorporate resolution language into these open negotiations. Managed care should educate the revenue cycle team about the negotiation process, timeline, and existing contract provisions. This background will allow revenue cycle to provide specific, actionable feedback leading into negotiations. Two key revisions that should be addressed in contract negotiations are language to provide adequate time to resolve denial appeals and amendments that require both payer and provider organization consent to revise contract provisions. Both of these revisions ensure the provider organization can protect its revenue from erosion due to denials volume increases. In addition, if payer organizations are unwilling or unable operationally to address major denial problems. then providers should negotiate higher rates to offset the revenue losses and/or the excessive administrative cost burdens.
Once contract negotiations are complete, managed care should develop a summary sheet of key contract terms for the revenue cycle team to reference during the follow-up process without needing to review the full contract.
A Team Approach for Improved Outcomes
Increased denial volumes negatively impact financial performance, staff efficiency, and provider and patient satisfaction. Though payer behavior contributing to these increases is unlikely to change soon, provider organizations should be vigilant in tracking denial trends, collaborating across administrative departments, and taking proactive steps to limit payers’ efforts to expand the scope of what they can deny. By coordinating a response that includes input from multiple departments to manage payers, provider organizations can improve revenue cycle outcomes and optimize the financial performance of their managed care contracts.
Need help?
Find out how ECG can help you navigate your payer contracts, relationships, and revenue cycle performance.

