
The rules are changing for healthcare providers with the shift from fee-for-service to fee-for-value. Factors that historically had little impact on how health systems structure care delivery, such as cost transparency and patient centricity, are becoming critical to provider organizations competing in the marketplace. At the same time, health systems are replacing traditional department-based clinical care; broader and more functional “service line” approaches bring together multidisciplinary clinicians and staff to focus holistically on patients’ health. Through the lens of five key themes, we’ll consider the critical factors driving successful health systems of the future and explore how future service lines might look different from the service lines of today.
Service Lines: Looking to the Future
Broadened Continuum of Care
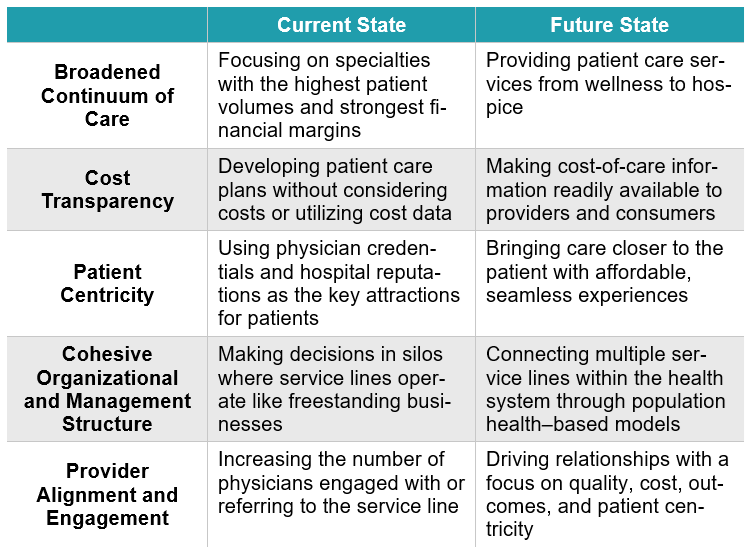
Current State—Although most healthcare does not take place in an inpatient setting, health systems and their service lines still largely have hospital-centric orientations. Many systems have historically used “service line” synonymously with “Center of Excellence” or “institute,” thereby focusing on specialties with the highest patient volumes and strongest financial margins (e.g., cardiology, neuroscience, oncology).
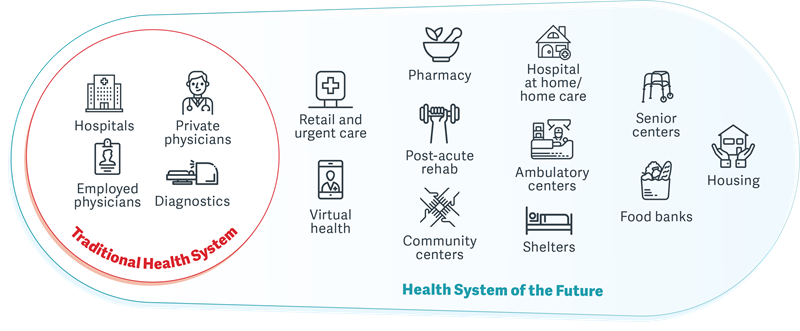
Future State—Service lines will develop a more holistic continuum of care in a market focused on clinical outcomes and patient preferences. Recognizing that clinical outcomes are often dictated by activities outside the control of healthcare professionals, future service lines will broaden to include patient care services from wellness to hospice, with an increasing use of home-based and virtual care. Likewise, an outcome-based orientation will require service lines to also address key determinants of health outcomes, such as behavioral health, food and nutrition, transportation, and housing.
Cost Transparency
Current State—”Value” is difficult to define and manage in healthcare, and we have little cost data. Very few provider organizations have robust cost-accounting systems. Thus, service lines and their providers are often disconnected from, and not at risk for, patient care costs. Providers, as a result, don’t usually consider cost a key variable when developing a patient’s care plan. Gaining popularity are bundles or episode-based payments, a reimbursement model that forces providers to consider the total cost of care; however, few service lines and health systems have embraced this model yet.
Future State—Providers will increasingly be at risk for the total cost of care. Service lines will need to help providers manage this responsibility and make informed decisions. Successful service lines of the future will supply providers with timely information so they can manage costs and improve outcomes for their patients. Unlike today’s wide variation in the types and quality of healthcare services provided, future service lines will eliminate unnecessary care by closely following standardized, evidence-based protocols. Service lines will be better able to predict the total cost of care for various services through the increased use of standardized clinical protocols and better availability of cost-of-care information. In turn, this information will be made readily available to healthcare consumers. However, achieving this level of standardization will likely require many service lines to adopt a narrow-network approach to their medical staff model.
Patient Centricity
Current State—Patients most often rely on physician credentials, hospital reputations, and established relationships when selecting a provider in the current healthcare environment. Without accessible information about quality or cost, patients largely follow a “rule out” rather than “rule in” standard when it comes to making choices about where and from whom they receive care, as well as the type of care they receive. In addition, patient care is usually organized around provider convenience (in terms of location, hours of operation, etc.) as opposed to patient convenience.
Future State—Healthcare of the future will be much more patient centric. Powerful, nontraditional healthcare players such as Amazon will continue to innovate and disrupt the business of medicine, and this will push provider organizations to design their services around the needs of patients. In recent years this shift has already started with the boom of more affordable and convenient retail and urgent care options. Service lines of the future must bring care closer to patients—when, where, and how they want to receive it. Patients will prefer options that offer affordable and seamless experiences over previous selection drivers, such as provider credentials or reputation, and this demand will force service lines to compete within a patient-centric environment.
Cohesive Organizational and Management Structure
Current State—Service lines today are often implemented in a way that creates silos within a health system. Without proper strategic planning and careful implementation, many systems let specialty-driven preferences create situations where service lines function as freestanding business units rather than cohesive entities that are part of a single system. Thus, many service line leaders are disconnected from important areas, both clinical and administrative, that are key to the optimal performance and management of their service line.
Future State—Effective health system management will replace traditional silos with cohesive, population health–based models. This will challenge system leaders to think about their organization’s service line strategy in a new way. There must be a “systemness” between service lines of the future, and service lines will need to be empowered (e.g., with more robust cost-accounting systems and financial analytics) to collectively better understand and improve the costs and outcomes of defined populations. As well, key aspects of infrastructure will need to be shared among multiple service lines, such as home-based care delivery models, virtual care, and behavioral health services. The concept of broadly sharing services among service lines will stretch the currently siloed organizational construct.
Provider Alignment and Engagement
Current State—For service lines today, provider alignment is all about increasing the number of physicians engaged with or referring to the service line. Often health systems are most intrigued by high-volume providers or those performing high-cost procedures. Rarely are factors such as the total cost of care, patient convenience, or outcomes considered when service line relationships are structured between health systems and physicians. As an unintentional result, there are often clinical and economic tensions among providers within a service line.
Future State—A focus on quality, cost, outcomes, and patient centricity will drive future relationships, and the criteria for partner selection will be materially different. The nature and structure of physician alignment relationships will also change. Currently, health systems typically enter economic relationships with physicians to align interests for a service line. In the future, economic alignment will be driven by the care model, and key elements may include the development or management of clinical pathways. For ambulatory service lines, there will be two types for health systems: owned and influenced. For owned service lines, the health system will continue to be engaged in the design and construct of the program. For influenced service lines (where much of the clinical care is provided outside the traditional health system construct), the system’s only role will be to convene the various clinicians and influence their decision-making. This evolution will also require physicians to become more than a single-specialty champion. Indeed, physician leaders of the future will need to be able to engage and build consensus across a diverse group of providers, including numerous nonphysician stakeholders (e.g., rehab, home health, wellness, social work).
Ready or Not, Change Is Happening
Service line shifts have already started within the healthcare industry. A holistic, patient-centric service approach can improve patient care and provide more visibility to monitor patient outcomes. The pace of change will vary from one service line to another, but insights from our whitepaper “Transformational Drivers in the Health System of the Future” point to common drivers that all health systems and providers will have to face soon.
Learn More About the Health System of the Future
Click on the button below to access the whitepaper.

