
A 750-bed hospital located in a major US city is filled beyond capacity—again. With no inpatient beds available, the teaching hospital is forced to not only board patients in hallways and procedural recovery areas, but also put its emergency department (ED) on divert, sending ambulances bearing nontrauma patients to other area EDs.
Scenarios like this are becoming commonplace for many hospitals, particularly in urban areas, which raises patients’ worries about access to timely services and hospitals’ concerns about quality, patient experience, and impact on the bottom line. This trend defies the projections of experts who warn that more and more hospital beds will sit empty as payers push for care to be provided in less costly settings. If inpatient utilization is trending downward, why are many hospitals scrambling to find additional beds?
A Shift in Utilization
Signs suggest that a large portion of utilization is not declining, but shifting. Oftentimes, observation patients are placed in inpatient units, which means fewer beds are available for those who are seriously ill and arriving via the ED or who need to recover from a surgical procedure.
From a facility and capital planning perspective, this growing trend presents a strategic dilemma: Should hospitals experiencing bed shortages invest in new beds?
Should Hospitals Invest in New Beds?
Hospitals should not add capacity that will be left unused in the next 5 to 10 years. As new care models become further entrenched, it’s likely that many of these observation patients will not be cared for in the hospital. For instance, as telehealth advances, patients could be monitored in their homes with proper outpatient follow-up. Alternatively, visiting nurses could provide support to patients recovering from surgery in their homes or a hotel setting. Hospitals must put the necessary foundations in place (e.g., care management structures, IT and digital capabilities) to safely care for patients in less costly settings. This is quickly becoming a financial necessity as alternative payment structures put providers at risk for a population’s total health costs.
Many hospitals need observation beds right now—and for the foreseeable future. Investing in a dedicated observation unit can result in a positive ROI. One study showed that hospitals without observation units could save $1,572 per patient on average if they were to put them in place. On top of that is the additional revenue obtained by freeing up inpatient beds for patients who need them.
The key, however, is ensuring that facility designs are flexible enough to adapt to future needs.
A Deep Dive into Utilization
Taking a deep dive into utilization data sheds further light on the issue. The decline in inpatient volumes is occurring as many have predicted. National inpatient use rates have decreased at a compound annual growth rate of 1.8% since the Affordable Care Act was signed into law. Inpatient admissions decreased from 114 per 1,000 population in 2010 to 104 in 2015. Research also shows that 24-hour-plus observation stays have increased significantly. Among Medicare patients, these stays grew 22.1% from 2011 to 2013. When examined together, what do these trends suggest?
According to a Medicare Payment Advisory Commission analysis, 40% of the inpatient decline can be explained by hospital patients being classified as under observation rather than admitted. This represents a sizeable proportion and helps explain why many hospitals are exploring the need to add capacity at a time when they had planned to downsize. From a strategic perspective, it’s important to note that 60% of the inpatient decline is not explained by the shift to observation. Thus, the trend toward outpatient care is still occurring, just not quite as fast as some statistics show.
Observation versus Inpatient Beds
While observation patients are considered outpatients by Medicare and other payers, they often spend time in the hospital, sometimes across one or two nights—and need a bed. But what kind of bed is necessary?
It helps to understand the different resource and space needs for inpatient versus observation beds. Inpatient rooms tend to be private, have generous footprints (260 to 300-plus square feet at contemporary standards), and typically have good-size bathrooms. Observation beds have less stringent requirements in terms of size and configuration. Hospital leaders certainly want to ensure a pleasant environment for observation patients, particularly given renewed focus on patient-centered care and satisfaction. However, since these patients are not as sick and usually have less complex conditions than typical inpatients, the accommodations do not have to be as comprehensive.
Flexible Facility Space
A solution for addressing capacity constraints is to develop a dedicated observation unit to care for short-stay patients. This allows hospitals to design processes that efficiently match the specific needs of these patients. In contrast, when observation patients are scattered around different inpatient units, they can get lost in the shuffle and end up staying in the hospital for longer than necessary.
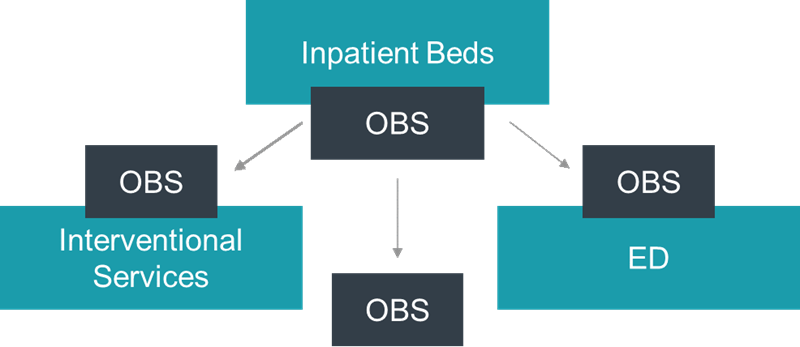
That said, not all observation patient types are created equal. Classification can vary between clinical decision made in the ED, general medical observation, and post-surgical extended recovery. Due to variations in staffing and patient needs, postsurgical extended recovery is usually accommodated in phase II recovery space. While clinical decision and general medical observation patients can be combined into one space for efficiency purposes, the right location for such an observation unit depends on physician coverage (hospitalists versus ED physicians), availability of space, and degree of need to free up ED treatment rooms versus inpatient beds, as depicted in the figure below.
Finding space for a new bed unit can be difficult for hospitals that are facing a capacity crunch, particularly if their campus is already densely developed. Additional options surface when the smaller space requirements of an observation unit are considered. Several hospitals experiencing recent capacity constraints have been implementing observation and extended recovery beds in quantities equivalent to approximately 10% of their inpatient bed capacity. This amount is dependent on market dynamics, scale of the hospital, and physician coverage, among other factors. In addition, observation beds should be considered in a business occupancy setting, especially for outpatient procedures, to further reduce the costs and space constraints typically associated with buildings that are designed for inpatient occupancy.
Take the example of Methodist Le Bonheur Germantown Hospital, a 309-bed hospital in Tennessee. Germantown’s campus is constrained and has limited expansion opportunities. There are plans to make use of a small piece of its site to build a two-level structure that would accommodate observation patients. The footprint is about 15,000 square feet, or approximately one-half of the size needed for an inpatient unit. It would effectively increase inpatient capacity by accommodating outpatients currently located in hospital units. The new development is adjacent to the ED and surgical suites, which would allow Germantown to easily convert the observation unit into ED or surgical prep and recovery space in the future.
Having a scalable facility plan like this is important, particularly as outpatient care models become entrenched. To help mitigate risks, it’s wise to design observation units with flexibility in mind. Building these units adjacent to EDs is typically a good strategy. Most observation patients originate from the ED, and the units can be readily converted to additional ED, procedural recovery, or outpatient clinic space to provide a logical expansion path for these services.
It can be challenging to balance near-term space needs with longer-term goals and projections. By designing scalable, flexible units for observation patients, hospitals can meet immediate revenue goals, provide timely care to their communities, and be primed for future demands.

