
In a widely anticipated statement, the Centers for Medicare & Medicaid Services (CMS) announced on November 16, 2015, the publication of a final rule that will require certain hospitals to participate in a bundled payment program for lower extremity joint replacements. The Comprehensive Care for Joint Replacement (CJR) program is designed to incentivize hospitals and contracted collaborators to actively share in reducing cost variation for joint replacements while improving quality and outcomes. These common orthopedic procedures can range in cost from $16,500 to $33,000, as noted by the announcement, and offer a significant opportunity for savings through reduced variation in utilization and more consistent care management.
As noted in previous ECG blog posts regarding the proposed rule, the program will utilize a retrospective model based on standard Medicare fee-for-service payments compared to a target price. The target price will include all Medicare Part A and Part B services for a 90-day episode of care and be determined on a rolling 3-year average, blending the specific historical utilization levels and regional averages. Savings or losses will be reported quarterly, but reconciliation payments will be adjudicated annually.
The proposed rule published in July 2015 garnered a significant number of responses from industry groups across the country, including the American Hospital Association and American Medical Association, many asking for changes to the program. The most frequently noted concerns were the mandatory nature of the program and the short time frame for implementation starting on January 1, 2016.
After reviewing an estimated 400 public comments, CMS made a number of alterations to the program, including reducing the number of affected metropolitan statistical areas (MSAs) from 75 to 67. Hospitals in the 67 MSAs will begin the program on April 1, 2016, three months later than the initially proposed January 1 start date. The agency also made some substantial structural modifications to lessen the burden on providers:
- The program will have risk-stratified MS-DRG target prices for patients with and without hip fractures. Utilization spending for patients with hip fractures can be nearly double those with-out fractures.
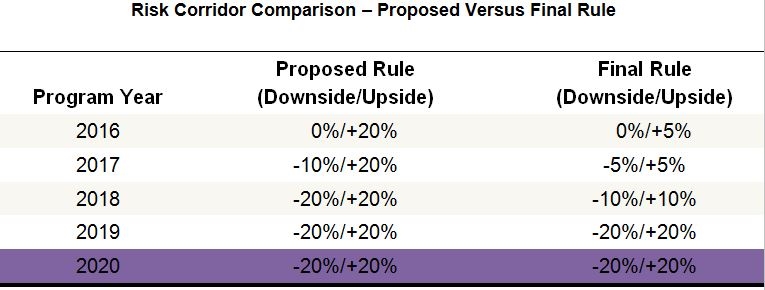
- The downside risk was reduced in Years 2 and 3 of the program. There is still no downside risk in the first year.
- To balance the reduced downside risk, the upside benefit will be reduced in Years 1, 2, and 3.
- The risk corridor for the 5-year program will now be as follows:
What happens now?
The timing and structural changes should not derail any current efforts to prepare for this program. Hospitals that have been working toward the proposed January start date are advised to continue in their efforts, while those that have not yet begun preparing get a little more time. Ultimately, with no downside in the first year, the April 1 start date represents a solid target but not a hard deadline for program preparations.
The final rule and details about the program structure can be found in the Federal Register. Check back in this space for future insights and strategies to address this and other upcoming bundled programs.

