
If your organization has completed a thoughtful analysis and determined that your incumbent system cannot be optimized, the next challenge is to plan and execute a successful replacement EHR implementation strategy.
The Game Plan
Replacing an EHR system is often more complex than implementing the original one. It’s critical to invest in up-front planning to define the business and end-user needs, implementation approach, data migration method, and technology integration strategy. To vet these areas, organizations should consider four components:
People
As with any complex project, the involvement and support of the individuals who are affected can ultimately dictate whether the outcome is successful.
- Organizational Buy-In – All users must understand how the new system will enable them to be more successful in their jobs
- Executive Leadership – Implementation cannot truly succeed if it is managed as an IT project and/or lacks clinical and operational leaders willing to hold people accountable for the success of the system
- Change Management – Acknowledge and leverage the valuable input experienced users may have while setting realistic expectations about what users will and will not have an opportunity to influence
Process
One of the most common mistakes made when implementing a replacement EHR is trying to recreate work flows optimized for the original system. Organizations need to:
- Perform thorough current-state work flow analysis of clinical processes
- Involve clinical staff and system application analysts in designing future work flows
- Thoroughly test work flows by a variety of users with quality initiatives and population health in mind
- Launch mock go-lives that simulate common processes from beginning to end
- Devise a strategy to transition staff from one system to the other
Technology
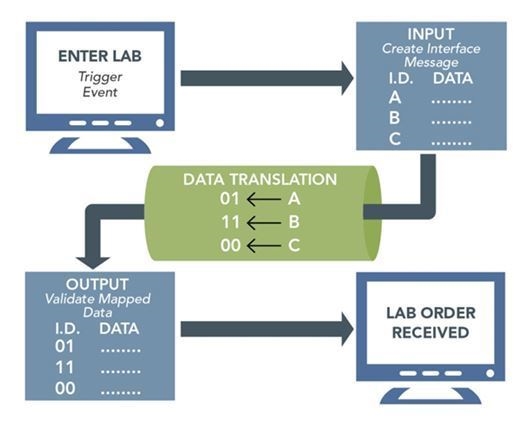
IT staff will most likely focus on the obvious technology impacts of the replacement system, including the often overlooked area of interfaces. Because a new system will involve new work flows and data mappings, the interfaces between systems should be reviewed in detail.
- Include an in-depth testing process that accesses each data element being passed between systems, any translation rules that may be applied to data, and triggers to pass off data at appropriate times
- Develop a data migration strategy to determine when data will stop flowing to the old system and start flowing to the new one. For example, if you perform your system cutover on January 1, does a lab result from a December 20 visit go into the new system or the old system?
Data
The replacement poses a new problem – there’s already a wealth of discrete data in the old EHR, and an organization may be tempted to move it all over. Treat the existing EHR as you did paper charts and ask the same question: What do you really need?
Consider converting:
- Active problem lists, allergies, medications, immunizations, and possibly patient history, last visit note, and lab results
- Long-term meaningful use, Physician Quality Reporting System (PQRS), or population reporting data required by your organization
Consider archiving:
- Data that is unlikely to be needed in routine patient care
- Data elements 3 years or older, including acute conditions and scanned documents
To learn more about successful EHR replacement, read the original article.

