
Patient-centered care delivery is effective healthcare provided in a manner that is convenient and accessible for patients. For healthcare systems, it also means that there is seamless access to a patient’s healthcare history across facilities. Moving to a patient-centered care delivery model has implications for healthcare providers’ infrastructure, technology, operations, facility design, as well as roles and responsibilities.
ECG considers patient-centered care delivery as a framework for achieving improved outcomes and quality performance, which are requirements for success in value-based reimbursement models.
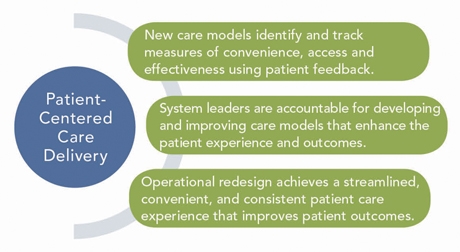
- Operational Redesign – Much of our healthcare facilities are designed to optimize staff and physician productivity, which often has quite the opposite impact on the patient experience. In some cases, there are limitations, such as how much sophisticated equipment can be relocated; however, other elements can be redesigned to improve the patient experience. Patients can contribute to operational redesign efforts in the form of focus groups and reports or surveys that track their care experience at your facilities. Operational redesign may involve changing the location of services, refining staff roles and responsibilities, and possibly moving to more team-based models for care providers.
- Management Accountability – Leadership should be held accountable for patient care delivery such that outcomes improve. Patient-centered care delivery models should continue to evolve to reflect improvements in treatment effectiveness, better access to care, and a customer-friendly environment. Accountability can be incorporated into management compensation tied to a set of measures designed to track the impact of new patient-centered care delivery models.
- Measurement of the Impact – Traditional measures of care from the patient perspective are often gleaned from satisfaction surveys. As IT systems progress, the ability to determine whether patients perceive care as convenient, accessible, and understandable also improves. Measures can be developed to track the patients’ care experience from their perspective, which can then be monitored on a regular basis. Meaningful use measures, patient satisfaction surveys (e.g., Press Ganey Associates, Inc.), and patient engagement measures are being enhanced to better understand the impact of patient care, in a patient-centered framework.
Action Items
Assessing your own work flow and patient experience is an effective place to start if your institution is interested in creating patient-centered care delivery models. We recommend the following key activities:
- Engage Patients: Care Design – Assemble patients into focus groups and routinely solicit their input on their care experiences. Ensure that feedback is translated into key considerations for operational and physician leaders. Gather patient input on access, convenience, way-finding, education, interaction with providers, etc.
- Engage Patients: Care Involvement – Create a culture in which patients are involved in a discussion regarding their plans of care. There should be evidence that each patient understands the recommended plan of care and documentation of a discussion of treatment options, as well as the patient’s ability and agreement to adhere to the plan of care.
- Address Operations and Facility Design – Review the patient care experience for typical visits. Consider revisions to facilities and operations that improve way-finding and minimize the distance within a facility that a patient must negotiate for routine visit interactions (registration, lab tests, diagnostic tests, clinics, etc.).
- Review Provider Work Flow – Engage providers in process redesign to improve the patient experience. Where possible, review the roles and responsibilities of staff to optimize effective engagement with patients throughout their visits.
- Develop Integrated Informatics and EHR – Design your IT infrastructure such that patients’ medical records are accessible to appropriate providers and staff across the system, as well as to patients through a patient portal. Informatics should enable personalized medicine, track outcomes and quality, and be able to incorporate patient input into their care and wellness plans. A well-designed informatics system will include the EHR; financial and claims data; operational and performance data; and research, quality, and outcomes data.

