More than any time in the last decade, health system leaders are being forced to reimagine the future role and delivery of primary care in their practices. Traditional primary care models are increasingly misaligned with modern consumer expectations and the preferences of self-funded employers, who are required to play a more active role in managing total healthcare benefit expenditures despite not wanting to.
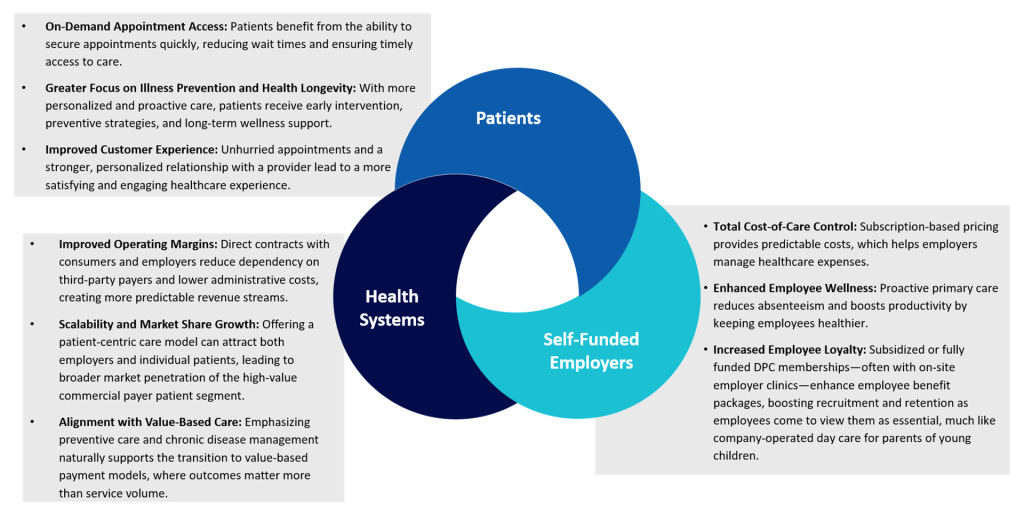
In response, physician enterprise leaders are exploring nontraditional practice models to adapt to market dynamics and modernize their primary care service portfolios. One such model is direct primary care (DPC), which is increasingly being adopted by health systems across the country due to its strong value proposition and use case for aligning care delivery and financial incentives across patients, employers, and provider stakeholder groups.
The Impetus for Change
Most traditional primary care practices still primarily rely on fee-for-service revenue models, which incentivize providers and operational leaders to maximize patient throughput and support large patient panels. The status quo model.
- Leads to a patient care approach that inadvertently focuses on symptom-based, reactive care.
- Produces poor on-demand access for both new and established patients.
- Does not support total cost of care containment goals for cost-conscious consumers and self-funded employers.
- Generates, on average, a medical group operating margin loss (i.e., net investment) of over $215,000 per physician.
A growing segment of US patients are insisting on accessible, on-demand, personalized primary care that focuses on prevention and wellness rather than episodic treatment. Simultaneously, self-funded employers face mounting pressures from rising healthcare premiums and unpredictable medical expenditures. The need for a change in the primary care landscape is evident.
The DPC Model
Enter the DPC model. DPC is a membership-based healthcare model where patients or companies (on behalf of their employees) pay a flat monthly (average of $80 per patient) or yearly fee that covers all primary care services, including office visits, preventive care, chronic disease management, and common lab tests. By eliminating third-party insurance billing, DPC practices offer more personalized care to smaller patient panels, typically between 600 and 1,200 patients; longer appointment times; and improved access to physicians through same-day or next-day visits. This model enhances patient satisfaction while reducing administrative burdens for providers, ultimately fostering a stronger doctor-patient relationship.
The DPC model is not a new concept—there are currently over 2,400 DPC practices and 3,500 DPC providers serving over 800,000 members nationwide—though historically, its adoption in health systems has lagged due to the business model’s operational and financial misalignment with fee-for-service reimbursement structures. In today’s healthcare environment, however, the model offers a compelling value proposition for patients, health systems, and employers looking to redefine the way primary care is delivered and experienced.
Planning for a Successful and Sustainable DPC Practice
To deliver on the value proposition of the DPC model, physician enterprise leaders will need to innovate care delivery in health systems, which have traditionally been slow to deviate from the status quo. Based on our experience, successful DPC operational planning in health systems will include the following activities:
- Determining DPC model fit within the health system and medical group strategy
- Understanding consumer demand, the employer partnership landscape, and existing competition
- Developing a scope of services, membership tiers, and associated pricing and billing approaches that are compliant with CMS laws and existing health plan contracts
- Customizing the care team model, provider recruitment approach, and provider compensation and incentive plan
- Developing an engaging and resourceful new-member marketing plan that incorporates employer outreach and engagement tactics
Why Innovate?
The transformation of primary care is not just a trend—it’s a strategic necessity. Health systems that embrace direct-to-consumer (DTC) and direct-to-employer (DTE) models can enhance patient care, secure predictable revenue streams, and lead the transition to value-based care.
Conveniently, many health systems already have strong relationships with regional employers through community development projects, philanthropic campaigns, executive participation on local organization boards, concierge medicine and executive health practices, and existing value-based care agreements.
Early health system adopters of DPC practices, such as Penn Medicine HealthWorks, are establishing market leadership in DTC and DTE practice models by realizing first-mover advantages with consumers, securing long-term employer partnerships, and differentiating their brand by offering modern and innovative patient-centric care models. Health systems that ignore the opportunity or delay the adoption of DPC models risk falling behind competitors that are making it a priority to adapt to evolving consumer and employer demands.
In a healthcare environment marked by rising costs and evolving consumer and employer expectations, adopting a DPC model within your health system’s portfolio of primary care services is a forward-thinking move that can deliver improved patient outcomes, enhanced operating margins, and stronger market share positioning. The time for innovation is now.
Edited by Emily Johnson

