
In Brief: Women’s health issues have made headlines in recent years. What’s in store for the coming year?
For years, two issues have dominated women’s health headlines: declining birth rates and the shift of services to the outpatient setting. But women’s health trends are evolving as new factors impact how, when, and where women receive care—and most critically, how health systems and payers should respond.
Below is ECG’s outlook on the market influences driving change in women’s health for 2023.
1. Unit Closures
Maternity, labor and delivery, and obstetric units are facing high rates of closure and consolidation. In the last six months of 2022 alone, more than a dozen hospitals have announced unit closures–largely because of staffing shortages and physician retirements. Recent reporting by the March of Dimes found that 36% of US counties are maternity care deserts—lacking any sort of maternity care for over 2.2 million women.
Implication
Consolidation of services is an opportunity for remaining providers and programs to enhance outreach services, expand their strategic footprint, and grow volumes.
2. Rising Birth Rate
After a decade of declining birth rates, the birth rate in 2021 rose by 1% and is anticipated to rise again in 2022. The historic decline in birth rates appears to have reached its trough.
Implication
Demand for OB services will stabilize generally with pockets of growth; flexing/tailoring services and providers to meet local market conditions will be critical.
3. Demand for High-Risk Services
Maternal age continues to climb, as the average age of motherhood in the US rose from 27.7 to 29.1 from 2010 to 2019. Paired with higher rates of comorbidities, this is driving a need for maternal-fetal medicine (MFM) and high-risk services.
Implication
Well-positioned programs will enhance volumes and financial opportunities by offering expanded program offerings for high-risk pregnancies, including MFM, perinatal diagnostics, imaging, and condition-specific support.
4. Medicaid Expansion
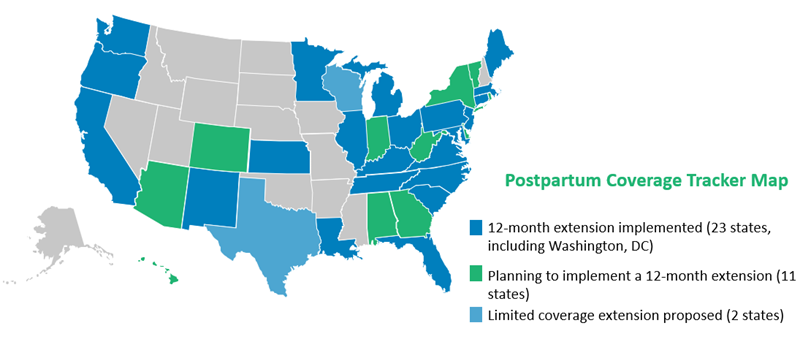
A majority of states have either implemented or are considering implementing a 12-month extension of Medicaid postpartum coverage, increasing access to services for women covered by Medicaid from 60 days postpartum to a full year.
Implication
Enhancing broader women’s health programs—urogynecology, gynecology-oncology, minimally invasive gynecology surgery, breast care, cardiac care—is key to new revenue, improved access, and better integration with the system. In addition, for systems that rely on birthing volumes to support disproportionate share or 340B funding, an additional 10 months of Medicaid coverage can help bolster these volumes by engaging the patient more broadly across the system.
5. Federal Quality Designations
Seventeen states currently feature maternal levels of care designations; federal requirements are now updated to include facilities that self-certify as Birthing Friendly and report quality metrics publicly.
Implication
While the reporting requirement is currently related to an attestation of participation in quality programming, the Birthing Friendly program will evolve with additional quality outcomes measures that will be tied to reimbursement. Being proactive will enhance very visible public benchmarks, patient experience, and most critically, outcomes.
What steps can your hospital take to meet patients’ expectations about the birthing experience?
Keep Your Facility Competitive


