Compensating physicians for inpatient OB services can be complicated by OB global codes that are ascribed to deliveries. The complexity often increases when evaluating inpatient labor and delivery services under varying contractual relationships that exist, often within the same organization (e.g., hospitalist versus non-hospitalist models; inclusion of advanced practice providers [APPs]; providers who are employed, contracted, or leased from an academic medical center).
To combat these challenges, it is important for provider compensation administrators to understand that there are numerous ways to compensate OB/GYN physicians and choose the approach that’s best for their organization and provider group.
Methodologies for Compensating Inpatient Delivery Services
There are three primary ways that organizations typically compensate physicians for inpatient delivery services:
- Global Code WRVU Attribution: WRVUs associated with a global code are split up and credited to each physician who provided a component of OB care.
- Laborist Coverage Compensation (in-house or unrestricted): A market call coverage shift rate is paid to the provider on call, regardless of the number of deliveries per shift. Depending on how this payment is structured it may also include some consideration for WRVUs, if employed, or collections, if contracted.
- Delivery Stipend: A one-time payment is paid to the physician who completes the delivery, and all outpatient services are credited separately.
Most organizations opt for the WRVU attribution approach for employed physicians, as it is the most equitable when defining compensation for actual services provided. Under the right compensation model and care environment, there is an opportunity to use this methodology for other OB/GYN providers as well (e.g., certified nurse midwife). But it is also administratively burdensome, and leaders need to fully consider the methodology’s benefits and challenges before adopting it.
A WRVU Attribution Policy Explained
Before considering whether a WRVU attribution policy is a good fit for your organization, it is important to understand how such a policy can work. Most often, WRVUs associated with global codes are split into three buckets: prenatal, antepartum, and postpartum. WRVUs are credited to the provider(s) who rendered each visit or procedure and then multiplied by a compensation per WRVU rate specific to the provider type (e.g., if certified nurse midwives are part of the care model, WRVUs may be respectively attributed and multiplied by a rate that is within FMV for that provider type).
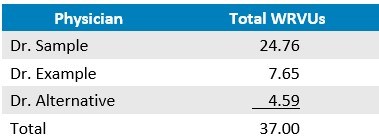
In the hypothetical scenario, Dr. Sample provides a vaginal delivery for a patient; 59400 is the CPT code assigned. This is a global code and is attributed 37.00 WRVUs, according to the 2024 Medicare Physician Fee Schedule (MPFS). Instead of compensating Dr. Sample for the entire global code WRVU amount, WRVUs may be attributed according to a formula such that each physician who provided professional services covered by the global code may receive WRVU credit, accordingly. Tables 1 and 2 show how WRVUs may be distributed to Dr. Sample as well as Dr. Alternative and Dr. Example, who also provided patient care covered by the global code.
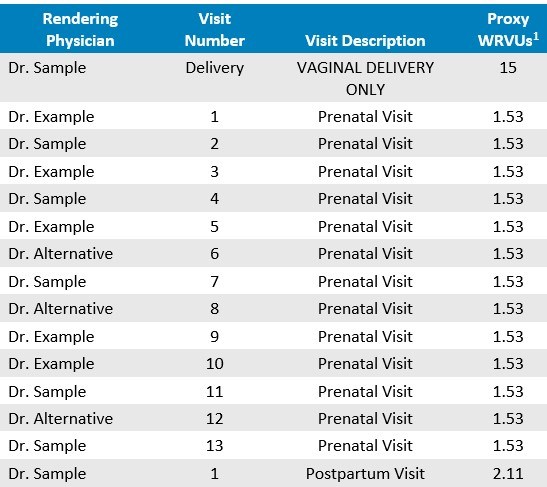
[1] CPT codes for single services may be used to establish WRVUs for each component of a global OB code. Alternatively, “proxy” WRVUs may be credited to each component of care such that the entire global code WRVU value is fully distributed. This example demonstrates the latter approach.
Weighing the Pros and Cons of a WRVU Attribution Policy
The next step for a healthcare organization is to examine its own structure, administrative resources and processes, and physician culture to determine whether a WRVU attribution policy is suitable.
The policy does offer organizations a variety of benefits. Physicians and administration alike will be able to transparently understand the work each physician is doing. This may result in the healthcare organizations experiencing the following:
- Productivity-Based Compensation: For organizations that generally pay physicians based on WRVUs, it may be important to align compensation with peers and support the culture of the physician group.
- Physician Satisfaction Associated with Equity: Physicians may feel more satisfied receiving credit for actual services rendered in lieu of credit being applied in a more vague manner (e.g., stipend), whereas a single physician may receive all WRVU credit for an OB global code or even no WRVU credit despite providing care throughout the OB cycle of care.
- Encouragement of Teamwork: Physicians will be encouraged to assist with the care of patients assigned to other physicians because WRVUs will be credited for such effort. This may support team-based care while also potentially preventing physician burnout.
All that being said, utilizing a WRVU attribution policy also presents challenges. Not every healthcare organization is equipped to implement this compensation approach, and leaders should be aware of several common obstacles:
- High Level of Administrative Burden: Physician compensation departments need to have adequate physician compensation staffing and technological processes in place for the policy to be successful and accurate. Implementation will also require educating physicians, educating billing departments, and facilitating collaboration across all of these involved stakeholders. This is important, as compensation will need to be calculated regularly and the policy will need to be continually reassessed in the context of any market updates (e.g., MPFS changes to OB global codes).
- Variability in the Financial Impact of Physician Compensation: Due to the variability of OB volumes and coding, healthcare organizations may find it more difficult to budget spend associated with a WRVU attribution methodology.
- Compliance Risk Considerations: If WRVU attribution policies are inaccurately designed or executed, there may be compliance risks. This is especially true if the total number of WRVUs attributed to a single global OB code exceeds the value of the global code itself. Furthermore, the fair market value (FMV) of physician services should be assessed based on actual physician services provided. This becomes difficult for organizations and internal FMV teams that are unfamiliar with the nuanced nature of compensating physicians for OB services.
Alternative Approaches
If an WRVU attribution policy does not seem reasonable for a healthcare organization, call compensation and delivery stipends may be considered as alternative approaches. Both may be easy to administer. The budgetary impact of call compensation will also be easily ascertained and consistent throughout the year.
However, call rates may not capture the burden of each shift, potentially decreasing physician satisfaction if the burden of each shift fluctuates. Alternatively, delivery stipends may also result in minimal or even no compensation depending on how busy the inpatient service is and may also encourage competition or one physician staying late to deliver a baby after their shift to ensure payment. Each of these approaches require a high level of collegiately among the providers to ensure equity and satisfaction while avoiding internal competition.
Choosing a Best Fit Approach
As organizations consider how to compensate for inpatient delivery services, a WRVU attribution policy serves as a potentially ideal methodology that can capture each component of professional physician services under a global OB delivery code, increasing transparency and providing healthcare organizations various advantages that serve to encourage physician satisfaction, recruitment, and retention.
As healthcare organizations weigh the pros and cons of the approach and consider alternatives, guardrails should be put in place regardless of the chosen approach to ensure successful administration and compliance.
Editor: Matt Maslin

