
Your organization has invested in and implemented an EHR system. Now, what exactly is your investment doing for you? In the current healthcare climate, organizations cannot afford to spend time, effort, or money on programs or systems that do not provide a competitive advantage or improve performance. While transitioning to an EHR satisfies regulatory and legislative requirements, organizations of all sizes also have a tremendous opportunity to maximize their IT investments and improve provider performance through metric-driven optimization.
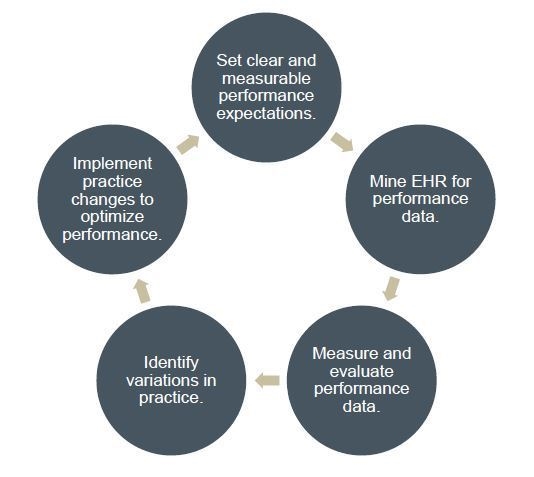
Metric-driven (or data-driven) optimization is the deliberate process of mining an organization’s EHR database for performance measures and using this information to drive continuous performance improvement throughout the organization. Ultimately, executing well-designed strategies to integrate EHR-captured data helps organizations identify and reduce practice variability, achieve incentive targets, maximize pay-for-performance awards, and coordinate patient care within and across organizations, among other benefits.
This article presents metric-driven optimization as an effective strategy for continuous improvement in areas such as practice efficiency, provider and patient satisfaction, and data quality. It also discusses some of the challenges and opportunities that organizations face following EHR implementation.
The Challenge
A metric-driven approach requires successful EHR implementation and adoption, coupled with a well-crafted plan for capturing and using data to enhance organization-wide processes and performance. However, despite the best of intentions, nearly three-quarters of EHR implementations fail. This failure is often due to an unclear vision, unrealistic expectations, and changes in technology without necessary changes in behavior.
The Opportunity
Organizations committed to data-driven optimization are positioned to drive meaningful change, realize quality goals, and facilitate sustained performance improvement. However, these benefits require an intentional strategy to usher organizations from EHR implementation through performance optimization, accounting for each step and challenge in between. Such strategies need to be specific to the organization and consider critical components, including instituting well-defined guiding principles for system adoption and data utilization.
A Compelling Case
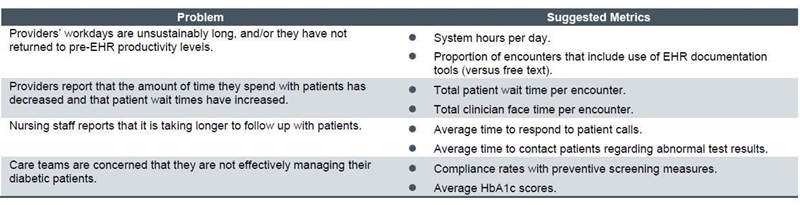
An implemented EHR does not guarantee a return. Organizations that fail to properly integrate and leverage EHR capabilities can quickly find themselves trapped in a post-implementation purgatory, paralyzed by disenchanted users and underwhelming provider performance – leaving these organizations with more questions than answers. Adopting a metric-driven approach to optimization, however, provides organizations with the ability to diagnose and correct problems by measuring and evaluating performance across specific metrics.
A properly integrated and fully utilized system can establish the foundation for significant and sustained organizational improvements, particularly in practice efficiency, provider and patient satisfaction, and data quality.
- Practice Efficiency – Fully utilizing an EHR system in a manner that optimizes provider and clinical support staff efficiency and productivity leads to greater adoption and, ultimately, helps validate an organization’s IT investment. In practices where the number of patient visits each day is not reflective of demand or desired provider capacity, providers are likely facing issues that limit or prolong their time at the point of care. There are myriad variables that influence provider productivity. However, when EHR-specific deficiencies threaten productivity, increasing system efficiency, providing proper training and IT support, and ensuring optimal leverage of system automation and nursing activities can boost provider capacity. Organizations that are able to increase provider capacity by an additional two patient visits per day (averaging $120 per visit in reimbursement) have the potential to increase revenue by more than $52,000 per provider each year. Across an organization with 70 full-time providers, this meager increase in capacity is worth more than $3.5 million in additional revenue.
- Provider Satisfaction – There is growing dissatisfaction with EHRs among users. The implementation of technological systems that frustrate or impede provider performance only contributes to the 11.5% provider turnover rate among advanced practice clinicians. 1 Losing and replacing a single provider costs a minimum of $250,000, but the actual cost often exceeds $1 million. 2 Reducing dissatisfaction, at least in part, by implementing technologies and processes that enhance provider performance increases retention. Increasing retention by just four providers equates to a $1 million to $4 million savings in costs associated with provider loss and replacement.
- Patient Satisfaction – Due to the amount of information and performance data available to the public, patients are quickly evolving into savvy healthcare consumers. With their choice of healthcare options, why would patients select and/or stay with a provider? Improving point-of-care interactions through timely, accurate, and actionable data and providing patients with the ability to access meaningful health information outside the clinical environment enhances the patient experience and contributes to a competitive advantage. Patient satisfaction not only drives loyalty but translates into greater reimbursement.
- Data Quality – Healthcare organizations are required to demonstrate their effectiveness by documenting, measuring, and reporting outcomes. Additionally, performance data is becoming increasingly comprehensive and sophisticated, extending beyond statistics traditionally drawn from practice management systems to include more provider-specific quality and care data captured in the EHR. Now that outcomes measures are directly linked to financial incentives and reimbursement rates, data quality is of particular importance, making accurate and actionable information an invaluable asset to organizations. Quite simply, having access to and insight into objective practice performance data increases opportunities to hit performance targets and achieve quality goals, as well as foster sustained performance improvement throughout an organization.
The Perfect Partnership
How an organization manages EHR integration and utilizes data to optimize performance, as well as whom it turns to for support in this process, plays a pivotal role in determining that organization’s success.
Balancing clinical, financial, operational, and technical considerations is an exceedingly complex task. ECG understands the challenges associated with implementing or replacing EHR systems and provides expertise in utilizing technology to drive sustained change.
Partnering with ECG helps organizations comfortably navigate the complexities of IT integration while providing a clear path toward continued quality and performance improvement.
Footnotes
1. Cejka Search, Inc., and AMGA 2012 Physician Retention Survey.
2. New England Journal of Medicine CareerCenter.


