
Up until a few years ago, electronic health records (EHRs) were optional for a majority of healthcare organizations. Early users created their own adoption criteria and other definitions of success. Some organizations achieved significant benefit in the form of streamlined operations, increased patient satisfaction, and enhanced coordination of care. Others had suboptimal results, but there were limited implications beyond frustration and possibly regret over a lack of return on investment. Today, however, the stakes are much higher. Not only has adoption been formally defined, but organizations are incentivized and ultimately penalized according to these increasingly challenging criteria.
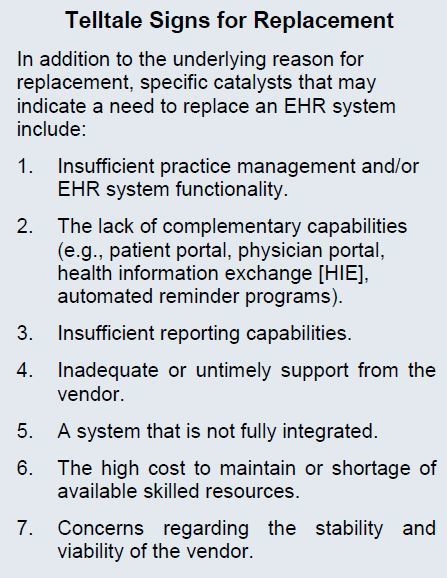
To that end, EHR systems and the vendors that provide and support them are being evaluated through a more critical lens by their existing client base. In some cases, organizations realize that the system in place does not meet their technical or work flow needs. Instead of being complacent and accepting the situation as fact, they are discussing more aggressive ways to address the perceived shortcomings. Other organizations are reaching the conclusion that the EHR no longer supports new strategic initiatives. The impetus for system replacement is typically related to one of two drivers: (1) high-level organizational change or (2) dissatisfaction with incumbent vendor products and services. In some cases, both of these factors may be involved.
This article describes the reasons that organizations should evaluate replacing their EHR systems and the critical steps to initiate the process. In addition, it will highlight the strategies for selecting and implementing a replacement EHR system.
Reason for Replacement: Organizational Change
Ten years ago, the technology needs of small and midsize independent practices were generally straightforward (as they relate to billing, for example). The interoperability requirements of stand-alone hospitals were also surmountable in most cases. In the last 5 years, the predominant organizational model has changed to one in which the majority of physician practices are owned by hospitals, and this arrangement is just one piece of a large physician network. These physician networks need advanced systems that support centralized billing efforts and clinical documentation for many different specialties. Hospital and physician practice systems alike must be able to send and receive information from disparate platforms within a single, yet complex, enterprise. Even those entities that remain independent have likely grown in terms of the number of providers, specialties, and service lines. Coupled with trends in mergers, acquisitions, and organic growth are industry changes such as value-based reimbursement, the medical home model, meaningful use, and ICD-10. All of these dynamics result in the need for more advanced technologies to support day-to-day operations as well as the strategic transformation required during the development and implementation of changes. Legacy systems quite simply may not be able to meet the business requirements of changing organizations.
Reason for Replacement: Dissatisfaction With Vendor Products
Replacing an EHR 5 to 10 years ago represented an incredible amount of time and money for implementation and maintenance. Such an undertaking was not only novel, it was nearly unthinkable. An EHR implementation is a time-consuming and challenging endeavor – and not something that an organization would voluntarily repeat unless absolutely necessary. The ability to convert clinical data can still be limited depending on the systems involved, and detailed patient account conversions are generally not recommended at all. But now that EHR replacement activities are more common, clients are more critical of their systems and their vendors, and replacement is considered a viable option. Some organizations have no choice but to replace because of products that have been sunset.
Best Practices for Success
Once a decision has been made to pursue an alternate technical solution, high-performing organizations do things differently – and better – based on their previous experiences. In our work with these organizations, we have observed that they take advantage of the opportunities presented during the selection process, demonstration stage, budgeting cycle, and contracting phase. An organization evaluating its second-generation EHR is an educated and sophisticated buyer; it should therefore create a list of required features and functions based on what has worked well and what is lacking in the current system – if anything, this list may need to be shortened or at least prioritized. The demonstration stage of the selection effort should be conducted using extensive scripts and scenarios based on what are known to be complex work flows that were either difficult to accommodate with the first system or that continue to be troublesome. The projected costs should include the unexpected items that arose during the first implementation. This time around, the new vendor contract should represent more than just a document stored on a shelf; for example, if one of the reasons for replacement is poor customer service, particular attention should be paid to the service-level agreement in the new contract to avoid experiencing these issues again.
A successful replacement implementation requires thorough planning and a greater level of technical and training support than is often anticipated. The eight most common issues confronted during the implementation of a replacement system can be addressed by ensuring adherence to the following best practices:
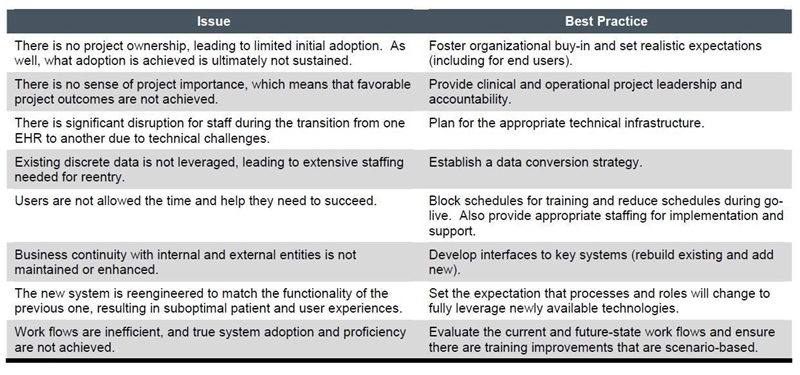
Two EHR implementations are one too many, and a third should most certainly be avoided. This means not just selecting the right replacement system and implementing it correctly but also designing an effective post-implementation methodology for monitoring and optimization to ensure that adoption is maintained as well as enhanced over time. System use should be evaluated at predetermined points in the process, such as 30 days after go-live and prior to any significant upgrades. Optimization efforts should be aggressively pursued when there is any indication of declining benefit, such as dissatisfaction, a lack of use, a large list of open support or enhancement requests, or a failure to meet stated objectives.

