
Recent changes to cardiology reimbursement have fundamentally altered the economics of an independent cardiology practice model and have led both cardiologists and hospital leadership to more seriously evaluate the benefits of physician employment. In the midst of an increasingly competitive marketplace, hospital leaders are under tremendous pressure to make quick decisions regarding cardiology employment, often negotiating poorly designed compensation arrangements in an effort to quickly secure their cardiologist networks. Although employment can serve as an ideal long-term strategy for cardiology service line development, a poorly executed compensation plan can impede its success. Organizations frequently experience unexpected losses due to diminished physician productivity and expensive compensation terms. Consequently, it is important to design a plan that incentivizes the right behaviors and maintains long-term financial viability. In our experience, the most effective compensation methodologies incorporate incentives that encourage clinical productivity, quality/care coordination, financial stability, and other variables aligned with broader cardiology service line objectives.
Successfully Navigating Cardiology Compensation
Compensation for physicians in cardiology-related specialties can be somewhat more complex and nuanced than other hospital-employed specialties. Despite significantly diminishing reimbursement rates for their services, cardiologists typically seek employment arrangements that maintain their historical income levels. To achieve these levels without substantial clinic losses, hospitals either need to offset this added expense through increased reimbursement or cost savings – efforts that are not always feasible. Additionally, cardiologists are increasingly subspecialized and frequently utilize unique compensation formulas in their independent practices that may not necessarily translate to the productivity-based models often favored by hospitals. While these types of arrangements may prove beneficial in incentivizing cardiology groups to engage in activities that support the hospital’s service line goals, such as community outreach, they can also introduce complexity into incentive arrangements.
Consequently, in determining an appropriate compensation model, it is important to choose a methodology that aligns with the organization’s broader strategies. If physician volumes are low, then a primarily productivity-driven model may be appropriate; however, if programmatic development is a more critical component of the cardiology service line, then a payment model that rewards physicians for non-billable activity may be more advantageous. It is also helpful to understand the degree of risk that each party is willing to entertain. Physicians generally prefer a high base salary, but a full income guarantee shifts volume risk to the hospital. Ultimately, each model has particular implications for group culture, physician recruitment, and an organization’s broader medical group compensation strategy, and all of these potential factors should be carefully considered when determining the preferred approach.
The models shown below represent the most common physician compensation arrangements, although characteristics from these various models can be combined to create alternative payment methodologies.
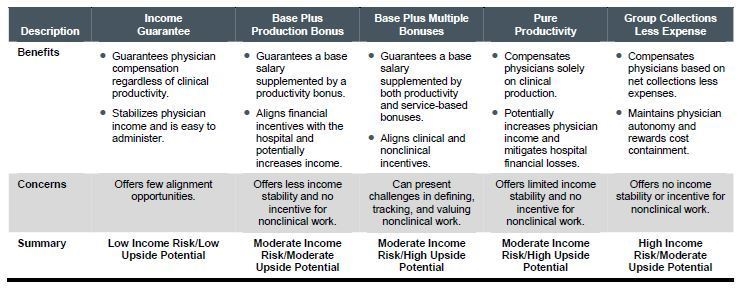
Regardless of the agreed-upon long-term compensation methodology, organizations tend to utilize short-term guarantees in an effort to mitigate physician concerns regarding their diminished productivity during the transition. A guarantee can serve as an effective short-term solution, but it is important to limit any guarantee in both duration and magnitude. Organizations frequently spend considerable time negotiating a rational compensation plan only to misalign incentives by providing a high, long-term guarantee.
Measuring Success Beyond Productivity
In the current fee-for-service environment, productivity-based compensation plans tend to be most prevalent. These plans are typically measured in work RVUs and utilize tiered payment rate structures that disproportionately reward high producers and provide strong incentives at the margin. However, many hospitals are seeking greater physician involvement in their broader service line performance efforts. Under a productivity model, physicians are not directly incentivized to perform nonclinical work. Therefore, incorporation of specific service line performance incentives that reward physicians for quality, citizenship, and other non-productivity related efforts can better support hospital objectives.
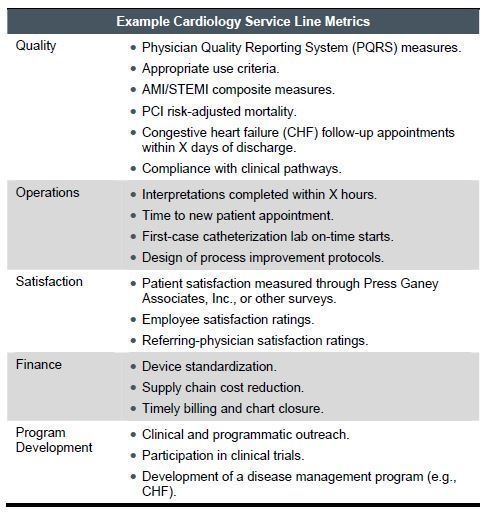
For most organizations, the percentage of service line incentives relative to total compensation remains small (i.e., 5% to 10%). Physicians are reticent to rely on hospital data, and hospitals do not necessarily have the resources to appropriately set baselines or monitor targets. Organizations that do utilize these types of incentives, though, quickly realize the overarching benefits to their cardiology service line performance – physicians are more engaged, care is better coordinated, and hospitals can recognize substantial cost savings. Consequently, there is a trend toward weighting these incentives more heavily in cardiology arrangements, sometimes as high as 25% of total compensation.
The table above shows example measures. The types of metrics will vary across organizations, depending on their particular programmatic objectives and payer contracting strategies; however, metrics should be based on “stretch” goals that are achievable, relatively easy to measure, and under the physicians’ control. Additionally, the number of metrics should be carefully chosen to ensure that total payment for each measure is at least roughly commensurate to physicians’ clinical compensation rates. Over time, it is likely that the percentage of service incentives relative to total compensation will grow, particularly as reimbursement shifts further to performance-based methodologies and physicians gain trust in the approach. Employment is an optimal way to prepare for these reimbursement changes, as it allows organizations to begin phasing in these incentives even before they are present in the payer market.
Positioning for Success
Over the next few years, the market will likely experience even further shifts toward cardiology employment, and the compensation plans that are developed will ultimately impact the ability of an organization to deliver coordinated cardiology care to the community. Therefore, it is important to structure a plan that is appropriately incentivized, balanced, and financially viable. In today’s rapidly evolving cardiology environment, it is a reality that many arrangements will be constructed but will not hold up to long-term payment changes and programmatic objectives. Properly structured, however, the employment of cardiologists can be highly beneficial to both parties and supportive of an organization’s broader strategic priorities.

