
Did you know PSAs were first developed by a surgeon? Well, sort of. In 1845, Dr. Horace Day invented the pressure-sensitive adhesive (PSA)—the first form of tape. Today, “PSA” is better known as an acronym for a specific type of hospital-physician arrangement, the professional services agreement. Tape has come a long way in the past 173 years—and it can be much stickier than Dr. Day’s invention. It’s time to make your PSAs stickier, too, to create long-lasting, mutually beneficial collaborations that help meet the needs of the communities you serve.
What Is a PSA?
PSAs provide hospitals and health systems a convenient and highly flexible mechanism to obtain services from physicians and achieve care coordination, access, and alignment goals. Under a PSA, a physician or medical group remains independent (i.e., not employed by the hospital) and provides professional services in the hospital or at a hospital clinic. PSAs are used to contract for hospital-based services (e.g., hospitalists, intensivists, anesthesiologists), emergency department coverage, and coverage at ambulatory clinics. They can range from part-time, narrowly defined, nonexclusive coverage with one physician to comprehensive, exclusive services with a large multispecialty group.
One advantage of the PSA model is the ability to tailor an arrangement to meet specific objectives and enable hospitals and physicians to achieve clinical and financial integration without employment. However, in many ways, the flexibility of PSAs also creates additional challenges in managing them to optimize their effectiveness. Frequently, PSAs are fragmented, one-off deals with no clear alignment with the broader strategies or priorities of the organization. PSAs are generally loosely managed or ignored until it is time to renegotiate and renew/extend the arrangement, and management often lacks the necessary coordination for effective PSA development and negotiation.
Regardless of whether your organization has 100 beds or 100 hospitals, more consistent, goal-
oriented, and integrated arrangements can be achieved by defining a clear vision for PSA relationships, developing PSA guiding principles and standards, and implementing a transition strategy to move existing arrangements to optimized PSAs.
Getting Sticky
Most PSA documents contain many of the same sections: obligations of each party, compensation, exclusivity, terms, termination provisions, and lots of legal mumbo jumbo. Occasionally, some of the hospital’s priorities will be captured in provisions of a PSA, but often what’s most important is overlooked, undocumented, and forgotten.
Today, health systems are pursuing value-based care strategies, and they need the collaboration of providers and associated medical groups to help them improve the quality and cost of services provided. On the path to value, health systems are building comprehensive provider networks that must not only demonstrate network adequacy and offer a full continuum of care but also enable organizations to compete on better outcomes and lower costs. Hospitals and health systems need to transition PSAs from transactional arrangements to more integrated and binding relationships that support their value-based strategies and build high-performing provider networks. They need sticky PSAs.
Sticky PSAs are arrangements that bind organizations more closely, promote a shared vision for ongoing collaboration, and align economic incentives and consequences. They create interdependency among otherwise independent providers through common goals, priorities, and infrastructure.
Through sticky PSAs, a health system is able focus on optimizing the performance of the provider network and increasing market presence, network stability, and competitiveness by creating accountability among medical groups, employed physicians, and hospitals.
Key Characteristics of Sticky PSAs
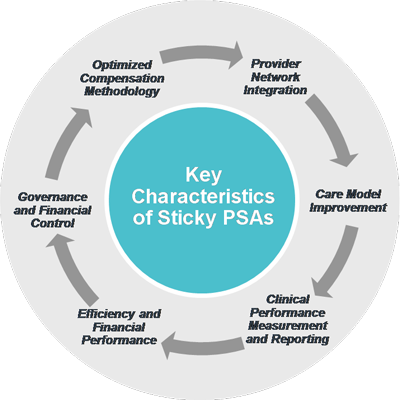
Sticky PSAs are characterized by six key elements: provider network integration, care model improvement, clinical performance measurement and reporting, efficiency and financial performance, governance and financial control, and an optimized compensation methodology. Figure 1 illustrates the six key characteristics of a sticky PSA.
Examples of incorporating sticky PSA characteristics are provided below.
Provider network integration
- Requires active participation by providers in organization-wide quality, cost, and efficiency initiatives
- Creates a high degree of interdependence and collaboration among the physicians to control costs and ensure quality
Care model improvement
- Identifies a common set of quality metrics and clinical initiatives for delivering patient-centric care across the care continuum
- Incorporates appropriate incentives for provider adherence to clinical standards, protocols, and patient care pathways and the achievement of clinical outcomes
Clinical performance measurement and reporting
- Requires PSA participants to track, measure, and share clinical and quality data
- Defines a pathway for the adoption of the health system’s electronic health record (EHR) and data aggregation tools
Efficiency and financial performance
- Identifies opportunities to reduce operating costs by centralizing contracts, leases, and purchasing, including physician preference items and outside services
- Monitors and manages revenue cycle performance and establishes minimum requirements for subsidy arrangements
Governance and financial control
- Ensures majority control over the physician enterprise or clinical program
- Controls physician participation on advisory boards that provide input on strategic and financial matters
Optimized compensation methodology
- Standardizes the compensation models for individual specialties/specialty categories and reduces variation where it makes sense
- Aligns incentives with payment models, long-term operational and strategic goals, and fair market value
The concept of a sticky PSA is not dissimilar to participation requirements found in agreements that bind clinically integrated networks (CINs). A CIN is a collection of healthcare providers, such as physicians, hospitals, and post–acute care specialists, working together to improve cost, quality, and efficiency and jointly contract with health plans. To participate in CINs, providers must sign agreements in which they commit to sharing data, advancing value-based care, and participating in quality improvement activities. If providers cannot meet the participation requirements (e.g., they can’t share data because they don’t have an EHR, they do not meet minimum quality thresholds), they may be excluded from the CIN. Participation agreements hold providers accountable to certain standards, drive collaboration, and maintain the integrity of the network. Sticky PSAs share many of these characteristics. The main difference is that sticky PSAs can be implemented in any organization regardless of whether it meets the high standards for being a CIN.
How Do You Get Sticky?
In a follow-up post next week, we will discuss actionable steps for implementing sticky PSAs at your organization, including what to develop, where to begin your efforts, and an overarching approach.

