
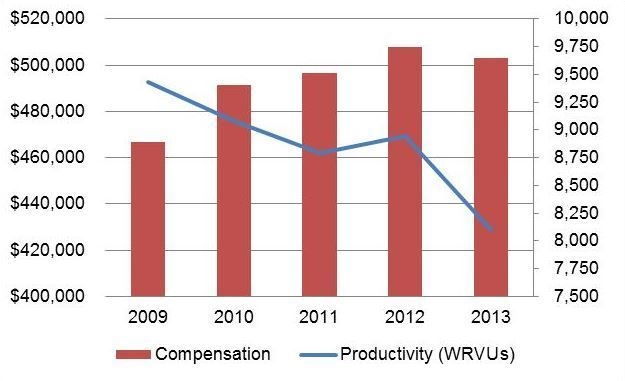
When you take a close look at the data from physician compensation and production surveys, you’ll find some interesting trends emerging in cardiology. For instance, a Medical Group Management Association (MGMA) survey reported that total compensation has increased 8% on average across all subspecialties since 2009. Meanwhile, productivity has dropped across all subspecialties by an average of 14% over the same time period, as shown in the table below. This diverging trend in benchmarking data presents significant implications for organizations tying compensation to market benchmarks, leading many administrators to question whether benchmarks are the right tool for measuring cardiology service line performance or calculating compensation.
Trends in Cardiology Benchmarks: MGMA All Specialty Average (Median)
So, what does this mean for the sustainability and market-competitiveness of your cardiology program, and what strategies should you be considering?
Baseline Performance Strategies
If your organization uses survey benchmarks for measuring performance or calculating compensation, it’s important to reduce the variability in the data and minimize organizational risk by employing a set of baseline risk mitigation strategies. Examples include using more than one survey, incorporating a rolling average of benchmark survey rates, and adding protective contract language regarding rate decreases/increases.
While these strategies are pragmatic for today’s practices, the growing complexity of cardiology raises an important question: Are WRVUs the right target to measure performance? If compensation levels are dependent on benchmarks, and the benchmarks do not reflect the realities of the market, then the continued practice of benchmark-based compensation needs to be reassessed. Organizations have to take a closer look at how value is defined (e.g., patient outcomes) and how that can be reflected in their compensation plans for cardiologists.
Future Performance Strategies
For those moving away from traditional benchmark-based approaches, there are hybrid models that incorporate a nonproductivity incentive component into a WRVU-based model. Under this scenario, a plan could tie 80% of compensation to productivity and 20% to nonproductivity measures (e.g., quality, program development). Examples of incentives include patient engagement, documentation, clinical measures, and practice efficiency. Additionally, some organizations are tying incentives to operating budgets, whereby physician compensation is dictated by the revenues and expenses achieved as a cardiology business unit. However, in setting the value thresholds (i.e., performance targets), it is critical to start with what an organization can actually track so that incentives can be monitored and executed.
In order to move discussions around value-based incentives forward, leaders will wrestle with the following questions: How does our organization currently define success and measure performance? How has this changed over time? How will we do so in the future? These are not easy questions, but they must be answered in order to develop cardiology performance evaluation tools that accurately reflect and align with the market and economic realities of your organization.
This post is adapted from a column that originally appeared in the December 2014 issue of CardioSource WorldNews, a publication of the American College of Cardiology.

