
The Centers for Medicare & Medicaid Services (CMS) is offering a second—and likely final—application period for BPCI Advanced, the new bundled payment model. Healthcare organizations that submit a nonbinding application by June 24, 2019, can participate in the second cohort and begin assuming risk for selected episodes beginning January 1, 2020. While organizations may be tempted to quickly complete the BPCI Advanced application and submit it as soon as possible, they should take advantage of the application period to gain an understanding of the current capabilities associated with the sections listed below—doing so will help them jump-start the process to operationalize many of the key components needed to implement BPCI Advanced.
- Organizational capabilities and readiness
- Care improvement
- Quality improvement
- Practitioner engagement
- Financial arrangements/Net Payment Reconciliation Amount (NPRA) sharing
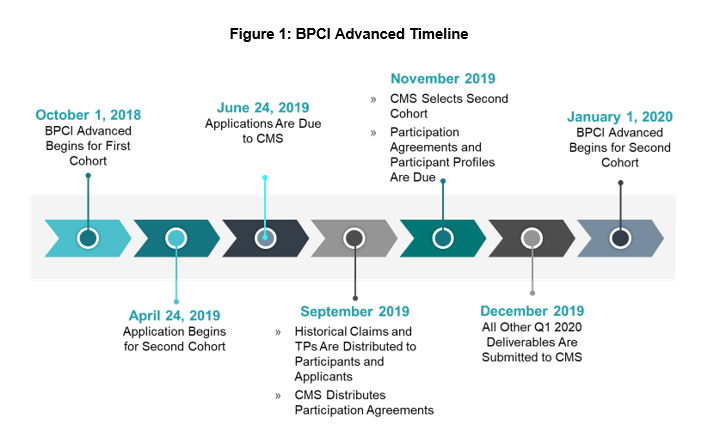
It takes time to implement a governance structure, develop care redesign strategies, and align physicians. Taking an inventory of organizational competencies may help expedite the episode selection process. Organizations that elect to participate in the second cohort are financially responsible for episodes beginning January 1, 2020, giving them only seven short months to apply to the model, analyze data, select episodes, and submit all other model deliverables, as demonstrated in figure 1. Therefore, using the application period to strategize will position organizations for success under BPCI Advanced.
Governance
Organizational Capabilities and Readiness
A dedicated bundled payment governance structure provides accountability and can serve as a framework to make decisions, align strategies, and achieve efficiencies. We recommend a bilevel governance structure that includes a steering committee and functionally oriented work groups (or Clinical Effectiveness Teams [CETs]), which will work in tandem to implement bundled payments. The inclusion of both levels of governance allows for multidisciplinary and effective collaboration. In establishing an effective governance structure, organizations should use the application period to:
- Identify steering committee and work group/CET members.
- Draft charters for the steering committee and each work group/CET, outlining their purpose, responsibilities, and short-term priorities.
- Educate stakeholders and develop a communication plan.
A formalized governance structure provides accountability and helps ensure that all bundled payment tasks are managed and completed in a timely fashion.
Care Redesign
Care Improvement
The BPCI Advanced model aims to encourage organizations to improve care delivery by adopting best practices, reducing variation in standards of care, and providing a clinically appropriate level of services. Under BPCI Advanced, care standardization activities often include the following:
- Care Design: Identify and document the services received by patients, as well as the timing of those services, from acute hospitalization through 90 days after discharge, ensuring that clinical protocols/pathways and order sets are also aligned.
- Care Coordination: Document the process by which high-risk, high-cost patients are identified and the criteria used to discharge patients to the next site of care.
- Care Transitions: Review and revise patient discharge instructions to ensure they provide clear and concise direction to patients based on a hierarchy of clinical issues.
- Readmission Reduction: Develop screening criteria to be used to identify patients who are at high risk for readmission.
With regard to care improvement efforts, organizations should use the application period to:
- Identify which care standardization activities should be prioritized and determine whether any activities can begin regardless of which episodes are ultimately selected.
- Develop a high-level implementation plan that outlines specific responsibilities, uses existing resources efficiently, and identifies any additional required resources in order to increase effectiveness and avoid duplicate work.
These preparatory activities will ensure that organizations have all the pieces in place to begin care redesign activities once episodes are selected in November 2019.
Quality Improvement
A crucial component of care redesign is the continual monitoring of performance. Therefore, organizations will need to identify key performance indicators/outcomes measures that will enable them to evaluate the effectiveness of redesign activities across the continuum of care for selected BPCI Advanced episodes. Given the complexities of many hospitals’ EHR systems, early stakeholder input in choosing the measures will give organizations time to develop reporting infrastructure prior to the start of BPCI Advanced. To aid in establishing effective performance monitoring, organizations should use the application period to:
- Develop and document data definitions for targeted metrics.
- Develop dashboards and reports that are automated and integrated across all sites of care.
The ability to monitor performance beginning January 1, 2020, will allow organizations to continually identify opportunities and course correct prior to the first reconciliation calculation.
Physician Alignment
Practitioner Engagement
One of the benefits of bundled payment models is that they provide organizations with an opportunity to engage physicians in improving care in collaboration with the health system and other providers. Organizations have the most success with bundled payments when physicians are involved in the program and take leadership roles to ensure favorable outcomes. Regarding improving physician engagement, organizations should use the application period to:
- Identify which physicians are best suited to be leaders or champions of the bundled payment programs.
- Review the status of physician engagement in key service lines and identify gaps that will need to be addressed in order to implement a bundled payment program.
An initial review of provider engagement during the application period will help organizations both evaluate their readiness for bundled payments and prioritize particular service lines that are the best candidates for implementing a bundled payment from the perspective of provider engagement.
Financial Arrangements/NPRA Sharing
BPCI Advanced allows for participants to share in the savings earned through the program, which serves as an additional incentive for physicians to achieve high-quality outcomes. Savings are generated when the actual cost of the episode is less than the target price set by CMS. These savings are pooled into the Net Payment Reconciliation Amount, which can then be shared between the health system and participating physicians per OIG regulations.
Organizations that have planned for this shared savings methodology during the application process will be well positioned for implementation at the start of the program. Identifying sharing partners can be a cumbersome and time-consuming process, so establishing a detailed plan for the financial arrangements up front will position organizations for success.
Planning Sets the Stage for Success
In our experience, organizations that use the BPCI Advanced application period to begin developing a governance structure, prioritizing care redesign activities, and engaging with healthcare providers will do well under this model. BPCI Advanced was designed to support providers who invest in care redesign to improve quality and reduce expenditures. Therefore, the more robust the structures in place, the better positioned organizations will be to manage episodes.



