Does it ever feel like the first step in any major initiative at your hospital requires the identification of a physician champion? If so, you’re headed in the right direction. At many forward-thinking hospitals, the appropriate physician champion for any initiative is obvious. These hospitals have established medical leadership structures that ensure physician input on key decisions and planning, facilitate medical staff support across the organization, and unite hospital administration and physicians behind common goals. They have learned the value of shared control and have proven that shared control is not an oxymoron.
The financial necessity of improved physician integration among our hospitals is clear. Hospitals recognize the importance of expanding beyond the walls of their facility and more closely aligning with physicians to improve clinical outcomes, coordinate care, and reduce the overall cost of providing care. Physicians are also seeking shelter from reimbursement cuts and the increased costs of running an independent practice.
For many hospitals, the most direct course to integrate with physicians is through physician employment. This is proving to be a successful strategy for many hospitals, whether they acquire large multispecialty groups or combine numerous small practices. But for many hospitals, large-scale physician employment is not a realistic option. Fortunately, the majority of the tactics that have proven successful in achieving integration with physicians are independent of the ownership of the organization and do not require major capital investments. Integration entails the evaluation and modification of practice patterns as well as the creation of interdependence and cooperation among physicians to control costs and ensure quality. Key elements to help achieve this integration are empowering physicians to share in service line management and creating a shared leadership model.
Empowering Physicians to Run Service Lines
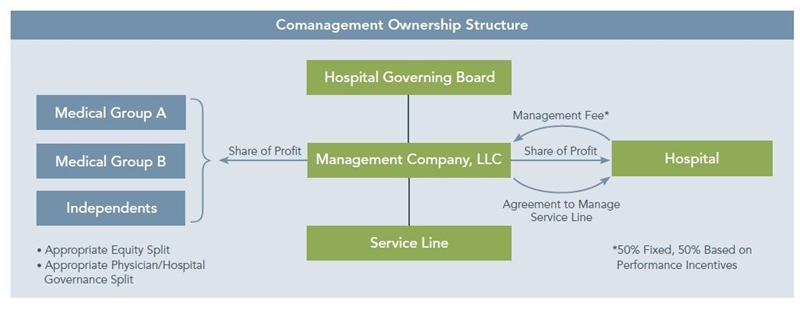
As part of shared leadership, comanagement arrangements are becoming increasingly popular because of their success in aligning the goals of the hospital and the physicians who impact the service lines’ costs, quality, and overall success. Under a comanagement model, the hospital and physicians jointly own a company that is contracted to manage the day-to-day operations and conduct long-term planning for a service line. (The management company could also be wholly owned by physicians.) Hospitals generally pursue these arrangements to:
- Enhance the delivery, operational performance, and quality of the service line.
- Facilitate the development of new service line opportunities.
- Align the goals of physicians and hospitals through the shared management of services.
Imagine the progress your hospital could make in lowering the costs of care, reducing readmissions, ensuring coordination among providers, and adhering to protocols if the physicians providing the care at your hospital were paid to make sure the metrics influenced by the hospital’s goals were achieved. Under a comanagement arrangement, a portion of the payments made to the management company are contingent upon the achievement of specific quality and efficiency measures. To ensure continued improvement in quality, measures can be refined on an annual basis, and compensation can be based on the outcomes.
Management companies are typically structured with physician investors and the hospital each holding a portion of the governing power of the management company. Ownership can be split equally or with majority ownership held by either the hospital or physicians. Comanagement arrangements often provide for one or more medical directors, an operations director, and an outcomes measurement coordinator. For an example, see the figure below.
Responsibilities of the management company may include the following:
- Development of the service line strategic plan and operating and capital budgets.
- Management oversight of the staffing, equipment, and supply/purchasing plans.
- Negotiation of the service arrangements, including hospital-based services (e.g., anesthesiology, radiology, pathology).
- Development of care protocols and quality management.
- Case management, including discharge planning.
- Creation of improvement policies and marketing strategies.
To enhance coordination throughout the service line and the continuum of care for each patient, we recommend that the management company assume responsibility for the entire service line – inpatient and outpatient. The following table summarizes some of the benefits of comanagement arrangements for hospitals and physicians:
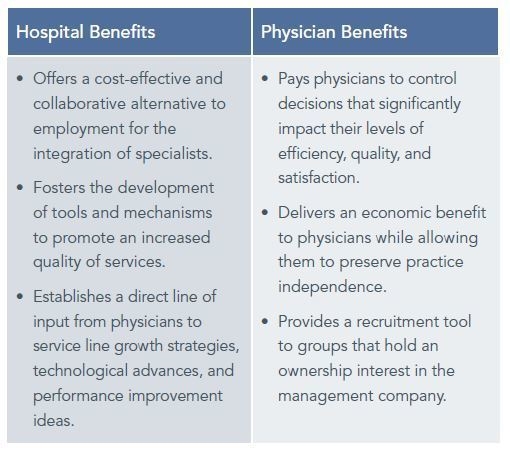
Finance executives often instinctively focus on opportunities to reduce costs through comanagement arrangements. However cost reduction is rarely a primary concern for physicians. Rather, physicians focus on opportunities to improve quality and the patient experience. Fortunately, the improved coordination, adherence to protocols, and other quality initiatives that engage physicians under a comanagement arrangement naturally result in reduced costs.
Creating a Shared Leadership Model
Physician leaders are best prepared to ensure quality and safety, achieve pay-for-performance goals, pursue service line development opportunities, and foster relationships with employed physicians and independent medical staff members. Developing an integrated patient care leadership structure often requires an iterative process that considers the organization’s needs and vision, evaluates options to determine the preferred structure, and considers patient care processes to devise a logical organizational structure.
Identifying Organizational Needs
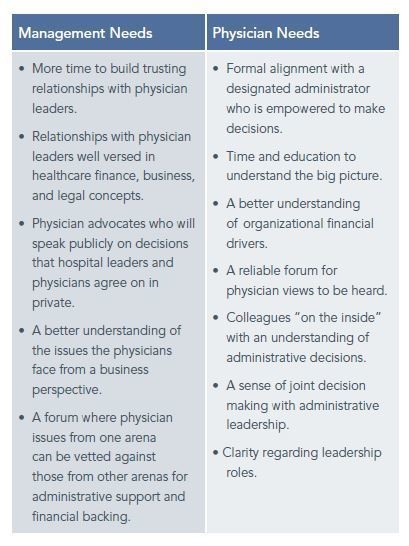
Poorly designed leadership models are a primary cause of ineffective communication between hospital administration and physicians. Finance and administrative personnel frequently become frustrated when physicians refuse to do what administration believes is best for the organization. But the physicians may have – and almost always do have – very good reasons to resist some of administration’s requests. The problem is that administration does not hear the perspective of the physicians and gain their input.
Additional needs of physicians and hospital administrators that should be considered in the process of defining the appropriate leadership structure are presented in the table below.
Evaluating Structural Options
After a common view of the needs of the organization has been established, principles should be developed to guide the evaluation of the structural options that will meet those needs. Three structural options to consider are depicted in the following graphic:
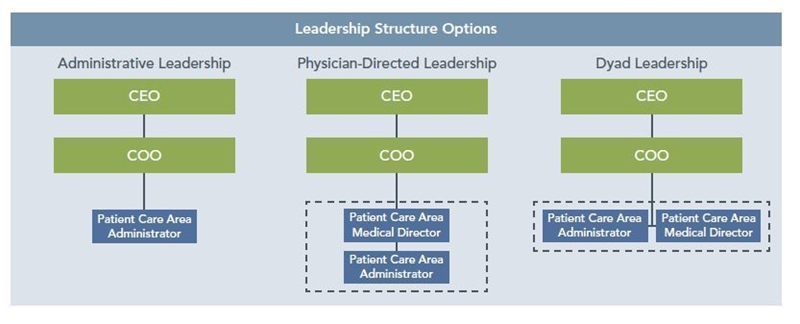
Administrative leaders may have a better grasp of the business aspects related to the organization and development of the patient care area. They are typically well trained to understand the organizational, operational, and financial implications of running a successful patient care area while evaluating growth opportunities. They are also easier to find and recruit than physician leaders and typically do not require the expense of a physician leader’s salary. However, this is the least integrative option and fails to meet the needs of most organizations.
Physician and dyad leadership models are gaining favor among leading hospitals. A cardiovascular service line management survey conducted jointly by ECG and Thomson Reuters found that 32 percent of Thomson’s 100 Top Hospitals for cardiovascular services use physician-led or dyad leadership models compared to only 8 percent among all other hospitals.
Physicians have a unique understanding of the healthcare environment, which may result in improved patient outcomes and compliance. The presence of physician leadership may also aid in the hospital’s recruitment and retention of top physician talent. Unfortunately, it often proves very challenging to recruit a physician leader who has business experience and understands the nuances of running a complex organization.
The dyad leadership model also presents its own benefits and challenges. The advantages of having both the clinical expertise of a physician and the business experience of an administrator may outweigh the added complexity that accompanies a dyad leadership structure. Each leader brings a specialized skill set to the organization, integrating a patient care and clinical focus with a hospital-business focus. Dyad leadership creates a more effective line of communication between administrative, medical, and nursing staff. However, the lack of a clear line of authority may create inefficiencies.
Organizing Patient Care Areas
In addition to determining the preferred leadership model, the organization of patient care areas and the reporting structure of the administrative and physician leaders must be established to create the shared leadership structure. Each patient care area may be composed of departments and divisions – each with their own physician/administrator teams reporting to the physician/administrator leaders. Variables that should be considered when organizing patient care areas and developing the new organizational structure include the
Graphic Footnote 1
- Revenue Impact – Total revenue should be used to provide an overview of the financial implications for each service area, as well as the level of administrative attention required.
- Physician Count – Physician head count is an indication of the level of oversight required to manage each service area. Physicians should be categorized by specialty and separated into proposed service areas.
- Staff FTEs – Staff FTE count can be used to determine the operational complexity of each of the proposed service areas.
- Number of Specialties or Subspecialties – Certain service areas may be required because of the complex nature of the specialty and/or large number of subspecialties that comprise it.
- Political and Cultural Influences – Third-party assistance is valuable to gauge the political and cultural influences that may impact the preferred structure and the obstacles that various options may lead to.
Many hospitals have already transitioned their organizational structure to optimize the performance of select service lines. This will aid in the move toward an organizational structure that integrates physicians with hospital administration and aligns with the overall combined vision and strategy of the hospital and its medical staff.
Where Do We Start?
The financial health of your hospital is contingent upon your ability to work with physician leaders to reduce costs and improve reimbursement by delivering high-quality services. To do so, your organization must create and maintain effective physician leaders, modify your organizational structure to incorporate physicians, and ensure that your organization is not confined within the hospital walls. Almost all of the high-impact changes you can make require the active participation of your medical staff. The most successful hospitals and health systems will be those that are run by physicians.
A clear understanding of the net market opportunity available to the organization is required to launch nearly any strategic initiative. When pursuing enhanced integration with physicians – whether it is with independent medical staff, part of an existing acquisition strategy, or within an ongoing employment situation – you need to create awareness about your market, the needs of your physicians and those you wish to attract, and who your customers are and what they want. This market insight must include all parties that will be involved in the integration process. You must bring physicians into your planning process and begin to establish common goals that can be pursued through a shared leadership structure and with physicians who are empowered to manage major service lines.
Footnotes
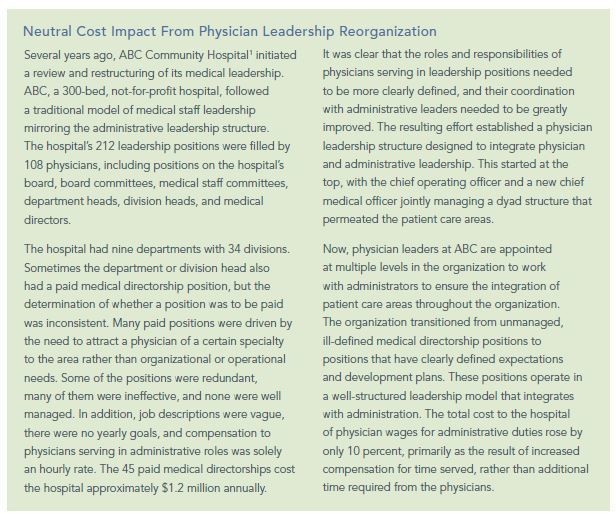
1. This is a pseudonym.

