
Despite rising costs and a shortage of cardiologists, cardiovascular (CV) programs remain among the top revenue-producing services in US acute care hospitals. And while there is a noticeable trend of migrating elective CV procedures to the outpatient (OP) setting, the emergency department (ED) remains a primary access point for hospital encounters.
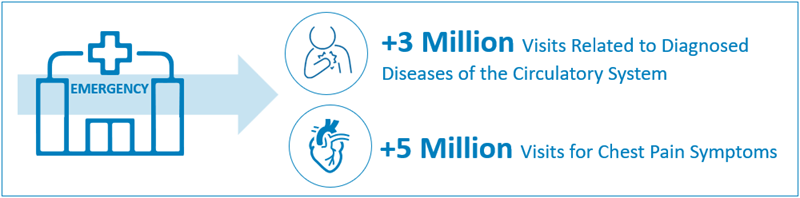
With more than 85% of the US population having access to a local or regional emergency STEMI system of care, an annual estimated 500,000 ED visits are dispositioned directly to a cardiac cath lab. Therefore, addressing the challenge of sustaining cardiology call coverage remains a top priority for CV service line leaders across the country.
Evolving Trends in Call Coverage
General and interventional cardiologists often have 24/7 on-call coverage requirements, and for some highly specialized programs, demand for call coverage is expanding to include electrophysiology (EP) and heart failure cardiologists. At the same time, workforce constraints are making it difficult to sustain adequate coverage:
- More than 60% of working cardiologists are now over the age of 55, and many older practicing cardiologists are unwilling to cover the required call.
- The US is not graduating enough net-new cardiologists to fill the gap for any level of access, let alone call coverage.
- A growing number of cardiologists are pursuing subspecialty fellowships and entering practice with an expectation of providing very limited call, placing growing pressure on general, noninterventional cardiologists to supply sufficient coverage.
While payment for on-call services in cardiology is not a new concept, it has historically been limited to interventional cardiologists. However, since the number of general cardiologists has decreased, many organizations are extending compensation to these providers to incentivize them to cover call. With current financial pressures, service line leaders must look for creative solutions to sustain call coverage.
Below are three foundational strategies CV program leaders can use to better manage cardiology call coverage over the longer term.
Strategy One: Be Proactive about Workforce Planning
With the cardiology physician shortage expected to continue over the next five years, it is critical that provider organizations maintain a comprehensive, multidisciplinary, three-to-five-year workforce plan. Executive leadership should collaborate with physician leaders to plan for service line succession, projected volume growth within existing programs, and future program development.
Specific to cardiology, we anticipate a continued trend toward subspecialization, meaning it will be important to develop guiding principles and objective criteria for how call will be managed for both general and subspecialty services. For example, at what point will it be necessary to implement a dedicated EP for call, and how will general call needs be backfilled?
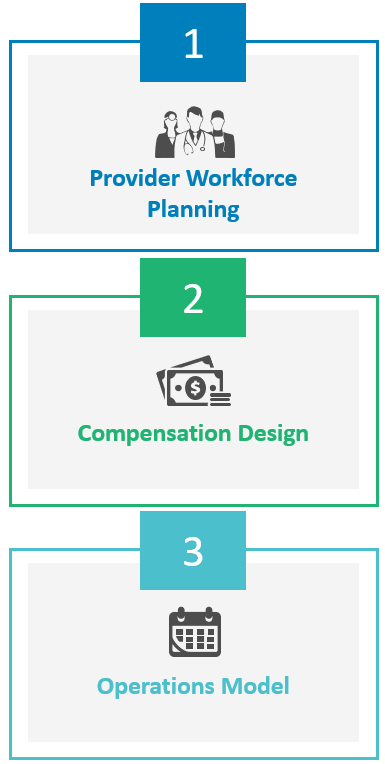
Strategy Two: Design a Contemporary Compensation Model
Since there will always be a need for cardiology call, most health systems are choosing to pay for this coverage, even if they haven’t historically.
For both private and employed groups, there is often a standard expectation of call coverage built into cardiologists’ base compensation, with additional payments reserved for excess coverage. In addition to meeting regulatory and legal requirements, a contemporary compensation model should be designed as follows to effectively manage CV service line call coverage expectations:
- Acknowledges call burden and sets clear expectations for responsibility and citizenship in covering call
- Clearly articulates the value of the total compensation package, inclusive of call coverage
- Embeds call requirements for every subspecialty in the overall compensation plan and establishes formal criteria to consider excess or specialty call coverage not already defined
- Includes thresholds, guidelines, and processes to manage growth (or contraction) in call needs
- Outlines procedural requirements and financial consequences for reducing call or leaving the call service altogether
CV leaders will want to maximize available physician resources, either through contractual or medical staff bylaw requirements, before incurring the cost of additional on-call services.
Strategy Three: Explore Innovative Operational Models
To help mitigate the burden of general cardiology call, we will need new ideas and strategies. Below areseveral operational models that may provide solutions. They can be tailored and/or mixed and matched to account for specific market characteristics and workforce supply issues.
Call, Consult, and Rounding Teams
Organizations can implement a shared-care model, under which rotating provider teams composed of general cardiologists, CV subspecialists with heavy call demand (traditionally interventional cardiologists), and APPs share the call burden. Optimal continuity of care can be achieved when teams rotate weekly, and this model supports efficiency, improved communication, and a high level of predictability for the cardiology team and referring physicians. The number of physicians and APPs should be based on the average daily demand for inpatient consults and follow-up visits. Upon discharge, the patient returns to their established cardiology provider or, if they don’t have one, becomes a part of the admitting cardiologist’s panel.
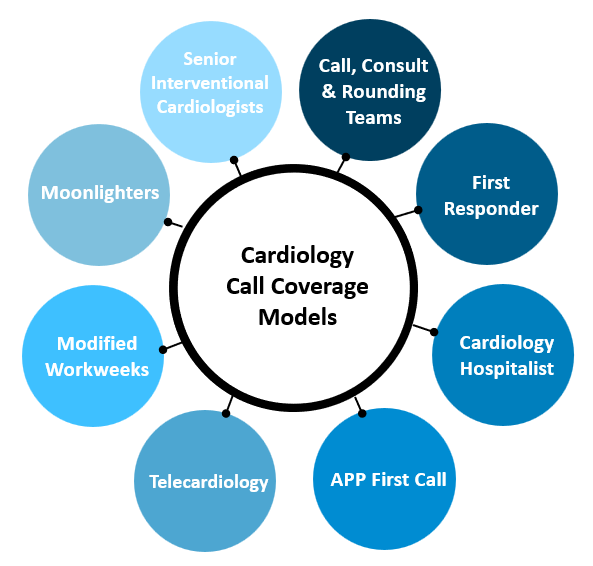
“First Responder” Coverage
Call responsibilities are assigned to a hospitalist or APP whose primary job is to cover call. First responders conduct patient assessments, perform histories and physicals, and order initial diagnostics with the goal of ensuring the patient is seen promptly to avoid care delays and then assigned to the most appropriate cardiology subspecialty service.
Cardiology Hospitalist or Nocturnist Program
This is a dedicated team of providers acting as full-time hospitalists and/or nocturnists for cardiology services. Team members may include cardiologists, internists, or PCPs with both interest and skill in the management of hospitalized cardiology patients and observation patients with suspected cardiac issues, as well as APPs. To support collaboration, communication, and care coordination, these teams are ideally members of the cardiology group.
APP First Call for Night Coverage
APPs may be assigned to handle the first call after hours for issues that can be managed by phone via established care pathways. While this team is backed up by a cardiologist if there is need for escalation, this option offers a safe and effective way to minimize the impact of after-hours calls on cardiologists.
Telecardiology
Managing call remotely may be possible via telehealth technology that allows providers to examine the patient and access diagnostic tests and imaging.
Modified Workweeks
Though less common in recent years, some organizations offer modified post-call schedules to mitigate the physical demand of high-volume call. As with any scheduling adjustments, careful planning is required to ensure clinic access is not disrupted or reduced.
Moonlighters
Moonlighters are often fellows who are completing their fellowship training nearby and provide part-time support, such as night and weekend coverage, to help reduce the call demand on cardiologists.
Senior Interventional Cardiologists in Slow Down
These cardiologists may be willing to accept a set schedule of general cardiology call to limit the overall burden for their colleagues.
When Care Is Critical, So Is Securing Call
As the rate of CV disease continues to rise across the US, CV services will remain a foundational program for hospitals and health systems, making it essential for these organizations to secure sustainable, effective call coverage arrangements. By using some of the strategies outlined herein, you can ensure your patients continue to receive the critical care they need.
About Our Team
If you need assistance in your program or you would simply like more information about call coverage arrangements, call schedules, call coverage compensation, or fair market value services, we have a team of dedicated professionals who focus on cardiology and call coverage arrangements who can help. Learn more about our CV services team.
Team-Based Care: Averting the Impending Access Crisis in Cardiology
In a team-based care model, all members of the physician-led team play an integral role in providing patient care.
Edited by: Emily Johnson


